PNAS:痴呆?帕金森?说不定是大脑缺了这个蛋白!
2019-12-06 转网 转化医学网
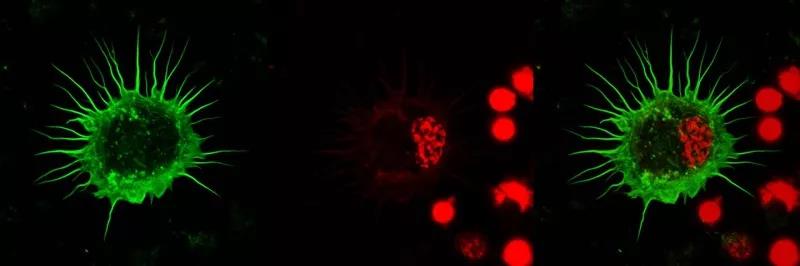
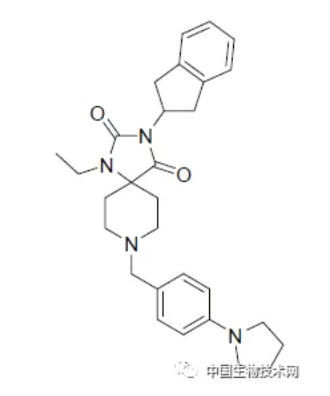
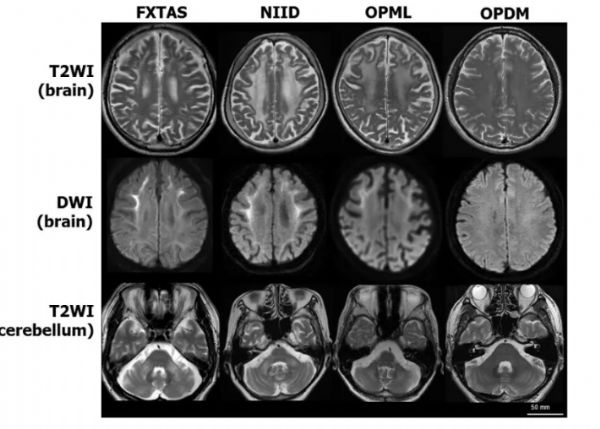
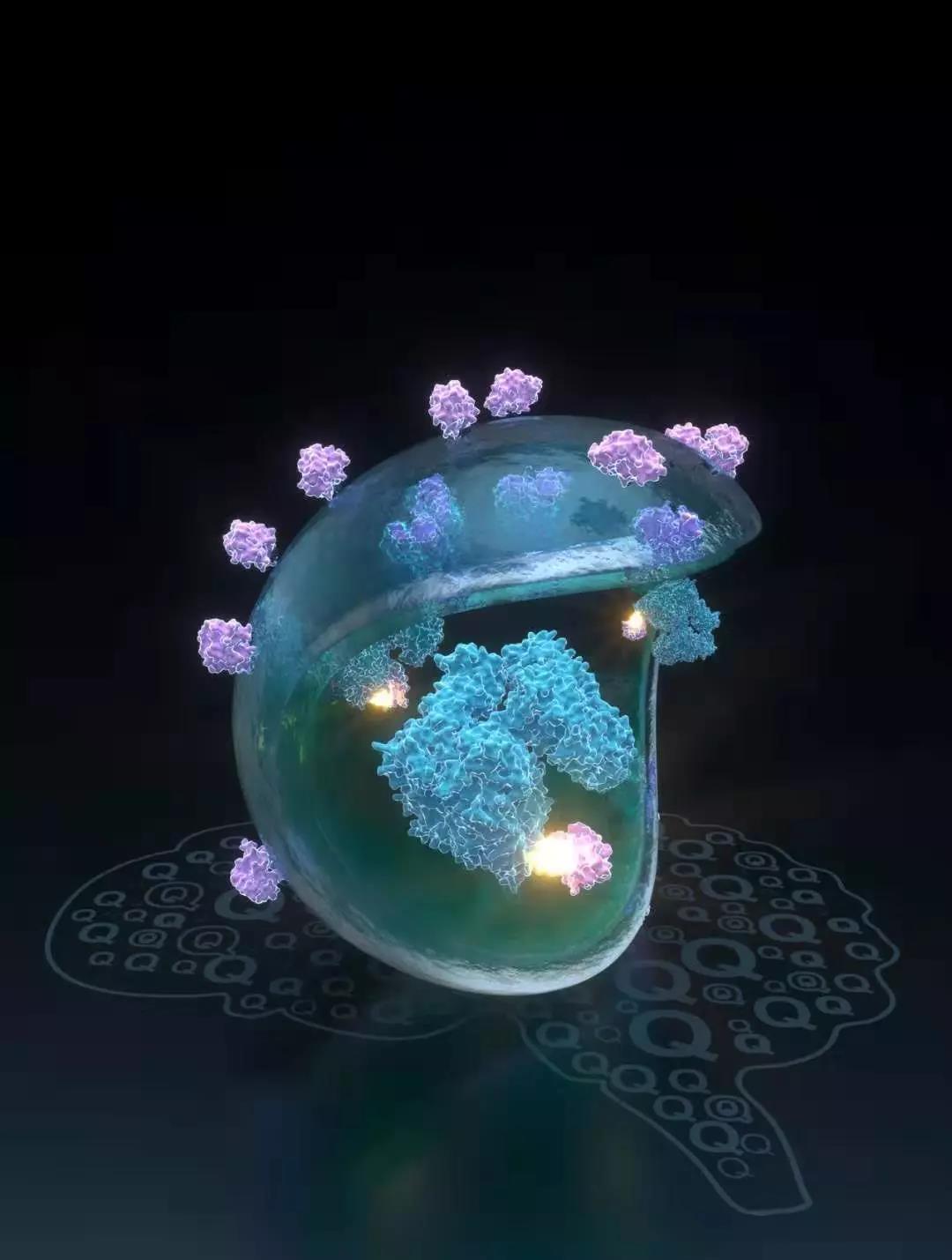
万事知其然才能知其所以然,但这些疾病的发病机制至今众说纷纭,有效的治疗方法扑朔迷离,研究长期桎梏于困境。近日,洛克菲勒大学的研究人员发现了造成神经退行性疾病患者大脑中异常蛋白斑块的罪魁祸首——缺失PI31蛋白。他们指出,这种蛋白的缺失可引发两大问题,不仅使异常蛋白的分解受损,还阻碍了神经元间的蛋白酶体交流,进而导致局部蛋白异常淤积,AD的β淀粉样蛋白和PD的α-突触核蛋白的大量聚集正是来源于此。泛
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PNAS#
35
老年人痴呆何药可用??
52
非常感谢好的研究
74
非常感谢好的研究
79
非常感谢好的研究
76
非常感谢好的研究
72
非常感谢好的研究
66