关节镜技术治疗急性创伤性肩关节锁定性后脱位1例
2019-11-08 钟名金 彭亮权 耿红荔 中华关节外科杂志(电子版)
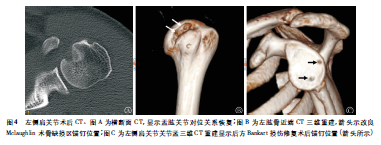
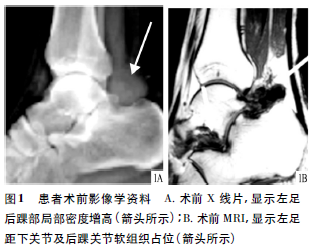
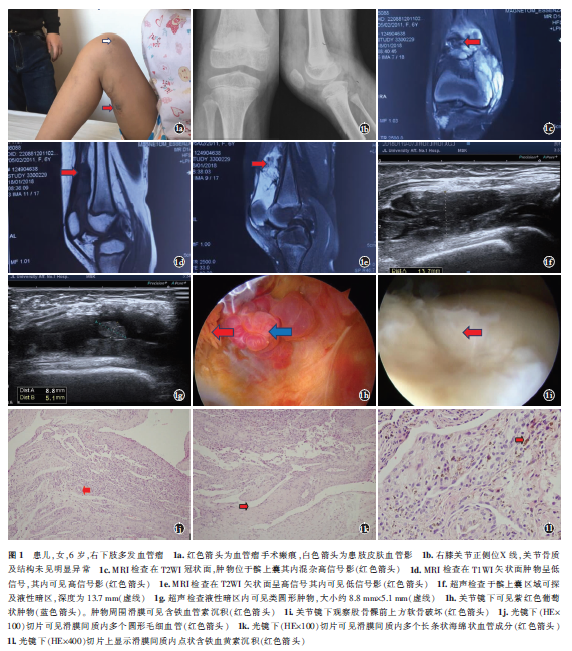
创伤性肩关节后脱位(TPSD)常因高能量外伤所致,在临床上非常少见,仅占肩关节脱位的2%~5%,因此很容易漏诊。正确诊断和及时治疗TPSD,特别是伴有反向Hill-sachs损伤的TPSD是骨科运动医学医生面临的一项挑战。笔者采用关节镜下改良Mclaughlin术(将肩胛下肌止点内移到骨缺损区)结合后方Bankart损伤修复术(将后方盂唇关节囊复合体缝合修补)治疗急性创伤性肩关节锁定后脱位1例。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#后脱位#
59
#创伤性#
34
#锁定性#
39
#创伤#
27
#肩关节#
53
#关节镜#
41
#脱位#
26