CANCER DISCOVERY:研究人员确定了致命肺癌的两个治疗靶点
2019-07-27 海北 MedSci原创
LKB1(STK11)肿瘤抑制因子中的突变是非小细胞肺癌(NSCLC)中第三最常见的遗传改变。 LKB1编码丝氨酸/苏氨酸激酶,其直接磷酸化并激活14种AMPK家族激酶(“AMPKR”)
LKB1(STK11)肿瘤抑制因子中的突变是非小细胞肺癌(NSCLC)中第三最常见的遗传改变。
LKB1编码丝氨酸/苏氨酸激酶,其直接磷酸化并激活14种AMPK家族激酶(“AMPKR”)。至今为止,许多AMPKR的功能仍然模糊不清,而且对LKB1的肿瘤抑制功能最关键的仍然是未知的。
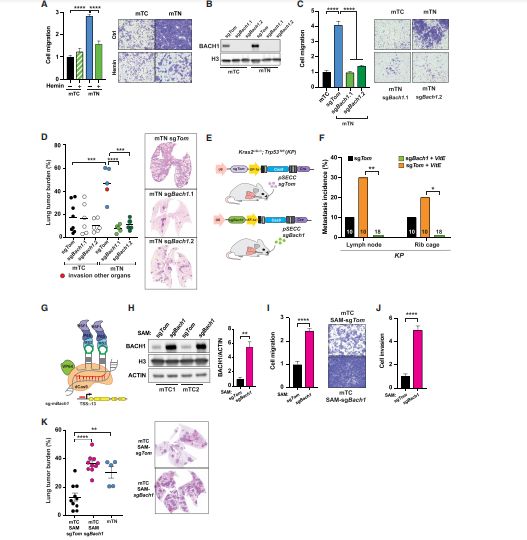
最近,研究人员将AMPKR家族的CRISPR和遗传分析结合在NSCLC细胞系和小鼠模型中,揭示了SIK亚家族令人惊讶的关键作用。
Sik1的条件性遗传损失揭示了Kras依赖性肺癌小鼠模型中肿瘤生长的增加,其通过丧失相关激酶Sik3而进一步增强。
由于SIK的大多数已知底物控制转录,研究人员进行基因表达分析,揭示了LKB1-和SIK1 / 3缺陷肿瘤之间共同的AP-1和IL6信号传导的上调。
SIK的底物CRTC2是这种效果所必需的,也是SIK损失的增殖益处所必须的。
原始出处:
Pablo E Hollstein et al. The AMPK-related kinases SIK1 and SIK3 mediate key tumor suppressive effects of LKB1 in NSCLC. Cancer Discovery, 2019 DOI: 10.1158/2159-8290
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#治疗靶点#
0
#cover#
43
#Dis#
24
#研究人员#
33
#ISC#
37