本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-03-24 佚名 肿瘤瞭望
肾癌及尿路上皮癌两项研究成果

细胞因子时代转移性肾细胞癌(mRCC)的中位生存时间(mOS)为12月左右1。靶向治疗时代提高至30月左右2-8。而近年来批准的乐伐替尼联合依维莫司再次将该数据延长了10个月左右9。如何贯序、联合以及寻找预测因子是目前迫切需要解决的问题。为此,我们报道了1例晚期Xp11.2染色体易位性肾癌的多学科、贯序治疗。
2018年第33届欧洲泌尿外科年会(EAU18)于当地时间3月16日在丹麦首都哥本哈根拉开帷幕。本届大会有多篇优秀的中国研究入选壁报展示,复旦大学附属中山医院郭剑明教授团队“应用中性粒细胞浸润预测肾癌TKI靶向治疗获益” 的研究也在其中。
肾癌是最常见的泌尿系统肿瘤之一,其发病率在全球范围内逐年上升,并呈年轻化的趋势;而目前对肾癌的发生机制仍不十分明确。大量研究表明,肾癌的发生、发展以及预后与其肿瘤微环境中浸润的各种免疫细胞之间交互作用密不可分。中性粒细胞是实体瘤浸润免疫细胞的重要组分,并且在不同的肿瘤微环境中表现出各自独特的表型。目前尚不清楚中性粒细胞在肾癌中的性质、功能、调节方式和临床意义。
肾癌约占所有成人恶性肿瘤的3-4%,是我国泌尿系统肿瘤第三大癌种。其中有将近一半的患者以转移性疾病起病或进展至全身转移。靶向治疗一定程度改善了晚期肾癌预后,但并非所有人都能从中获益,部分患者对靶向治疗可发生耐药。提前预测患者对靶向治疗的敏感性有助于更精准地药物治疗选择。
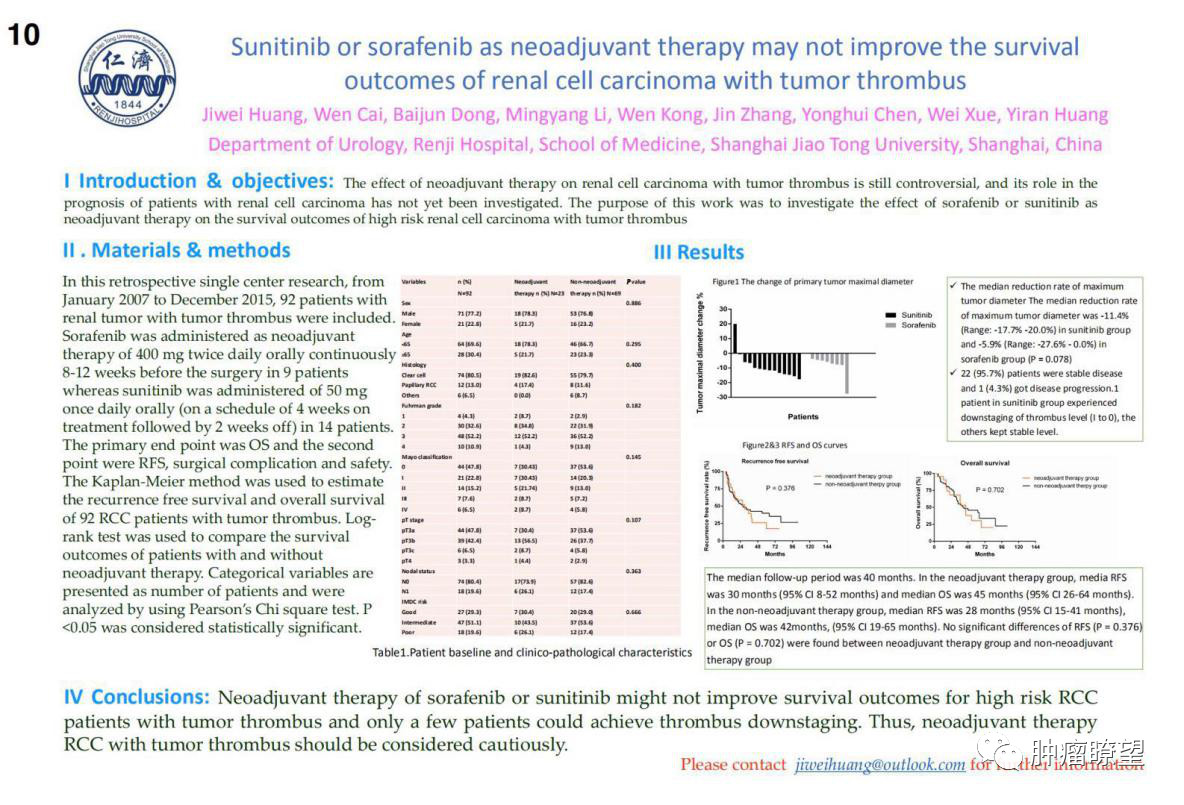
肾细胞癌是泌尿系统三大恶性肿瘤之一,发病率逐年上升且患者有逐渐年轻化的趋势。因此,肾脏肿瘤正日益成为威胁国人生命健康、增加国民经济负担的重大健康问题。
研究认为,相比于舒尼替尼,纳武单抗+伊匹单抗可大幅延长晚期透明细胞肾癌患者生存期


梅斯医学MedSci APP
医路相伴,成就大医
#研究成果#
26
#EAU#
26
#上皮癌#
30
学习一下谢谢
58