Int J Impot Res:西地那非在前列腺切除术后勃起功能障碍中的相关分析
2019-03-19 AlexYang MedSci原创
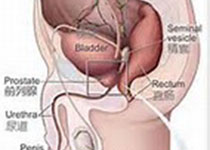
勃起功能障碍(ED)是根治性前列腺切除术的常见副作用,甚至在神经保留操作中也存在。为了减轻上述问题,被称为阴茎重建的计划已经开始进行。在上述问题中,最为常用的方法是在患者术后进行西地那非治疗或者PDE5抑制剂治疗。该方法基于一种理论,即这些药物可能能够增加阴茎氧化作用并提供抗凋亡因子(主要是NO和cGMP),从而保护阴茎组织在术后一段时期内神经功能减弱。预临床研究确认了西地那非在治疗ED中的作用,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
21
#前列腺切除#
26
#勃起#
30
谢谢分享学习
67
#功能障碍#
34
#勃起功能#
26
#MPO#
20