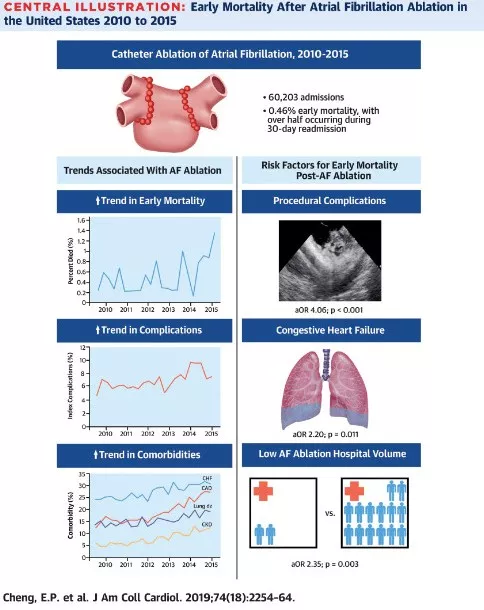
美国每200例房颤消融就死亡1人!JACC研究:合并心衰的患者死亡风险高
2020-01-19 xujing 中国循环杂志
美国一项2010~2015年间入选60203例的全国性研究显示,每200例房颤射频消融术后,就有1人死亡,大多数死亡发生在30天再入院期间。有手术并发症、心力衰竭和医院房颤消融量少是早期死亡率的预测因素。导管消融术是治疗房颤的一种越来越常用的治疗策略,在许多重要的临床试验中,如CASTLE-AF和CABANA都显示了其有效性和安全性。研究发现,从2010年到2015年,消融后早期死亡率从0.25%
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
32
#房颤消融#
54
#患者死亡#
35
#死亡风险#
34
#ACC#
33
#消融#
30
房颤,临床上碰到很多哦
38