Blood:老年人确诊癌症前5个月,动脉血栓栓塞风险增高
2019-01-11 MedSci MedSci原创
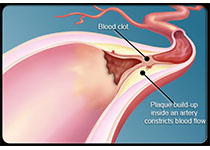
中心点:在748662位参与医疗保险的人群中,确诊癌症前一年动脉血栓栓塞事件的风险增加69%。动脉血栓栓塞事件的风险于正式诊断癌症前5个月开始增高,并在前一个月达到高峰。摘要:癌症患者动脉血栓栓塞事件的风险升高;但目前还不明确风险是从什么时候开始增加。Babak B. Navi等人对确诊癌症前的动脉血栓栓塞事件风险进行评估。研究人员从数据库中筛选出374331位年满67岁的于2005-2013年间
在748662位参与医疗保险的人群中,确诊癌症前一年动脉血栓栓塞事件的风险增加69%。
动脉血栓栓塞事件的风险于正式诊断癌症前5个月开始增高,并在前一个月达到高峰。
摘要:
癌症患者动脉血栓栓塞事件的风险升高;但目前还不明确风险是从什么时候开始增加。Babak B. Navi等人对确诊癌症前的动脉血栓栓塞事件风险进行评估。
在癌症确诊前的360-151天,两组的30天动脉血栓栓塞事件风险相近。从癌症确诊前150-1天,癌症患者的30天动脉血栓栓塞事件风险要高于匹配的对照,而且随着癌症确诊时间的临近,风险逐渐增高,并于癌症确诊前1个月达到高峰;在癌症确诊前1个月内,2313位(0.62%)癌症患者诊断出动脉血栓栓塞,而对照组仅413位(0.11%;优势比 5.63;95% CI 5.07-6.25)。
综上所述,老年人确诊癌症前150天,动脉血栓栓塞事件的风险开始增加,并于前30天达到峰值。
Babak B. Navi, et al. Arterial thromboembolic events preceding the diagnosis of cancer in older persons. Blood 2018 :blood-2018-06-860874; doi: https://doi.org/10.1182/blood-2018-06-860874
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉血#
27
#动脉血栓#
39
#增高#
32
#增高#
37