Nat Immunol:中山大学揭示lncRNA调控肿瘤免疫新机制
2018-09-18 朱汉斌 林伟吟 刘文琴 科学网
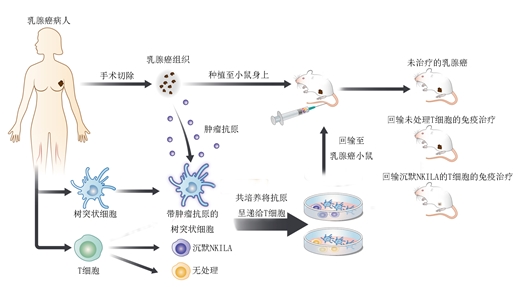
记者从中山大学孙逸仙纪念医院获悉,该院宋尔卫、苏士成教授团队发现了长非编码RNA NKILA能促使肿瘤特异T细胞被诱导凋亡,以至于不能开“猛火”攻打肿瘤。研究提示,可在体外将T细胞中的NKILA敲除,从而保证回输到体内的T细胞的“火力”,增强免疫治疗的效果。相关研究9月17日在线发表于《自然?免疫学》杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
22
#CRN#
28
#lncRNA#
32
#中山大学#
27
学习了谢谢
76
治疗淋巴瘤、黑色素瘤等方面,免疫治疗效果显著。然而针对乳腺癌等实体肿瘤,免疫治疗疗效仍比较微弱,
77
厉害了!
61
学习了
80
厉害
59