Circulation:动脉粥样硬化中的保护性CD4 T调节细胞的致病性转换
2020-10-01 星云 MedSci原创
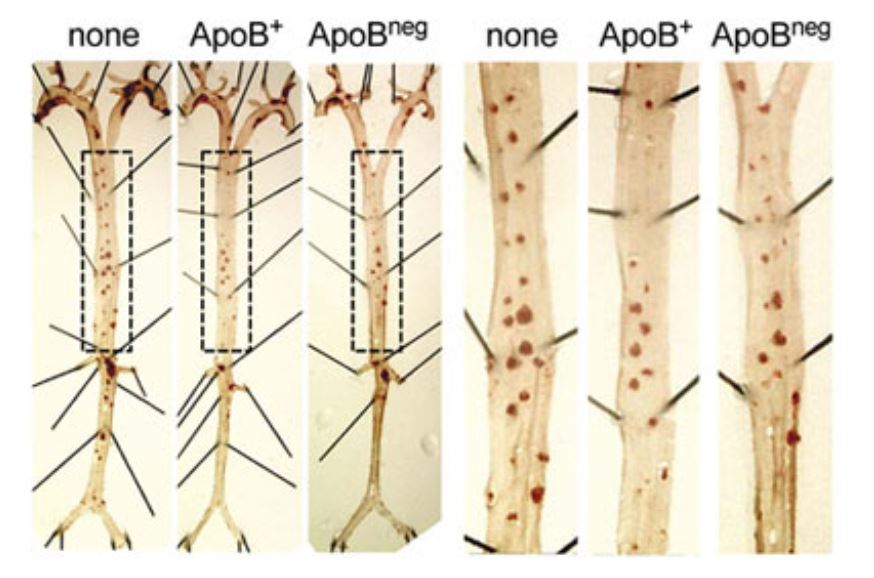
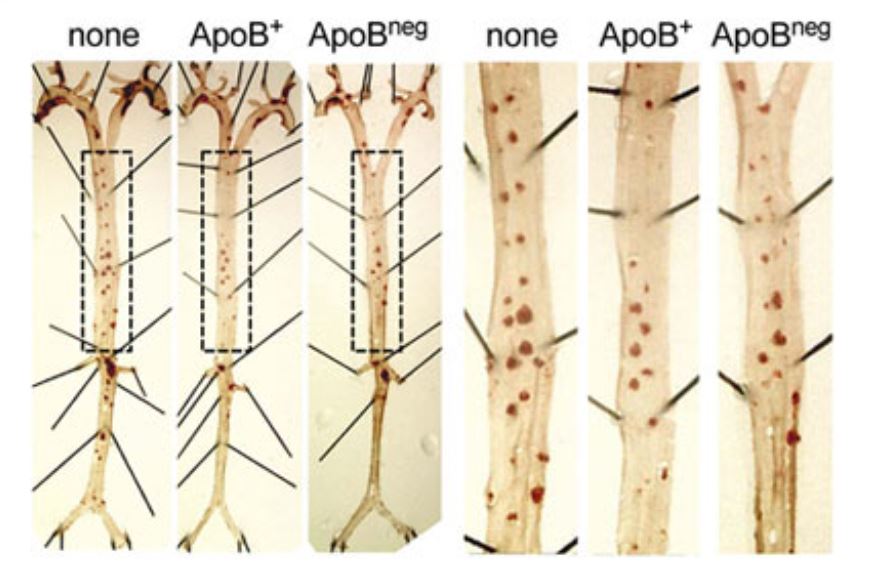
在伴随动脉粥样硬化的炎症反应过程中,自身反应CD4+ T辅助细胞在动脉粥样硬化斑块中积累。载脂蛋白B100(apoB),低密度脂蛋白的核心蛋白,是一种自身抗原,可驱动产生致病性1型T-辅助 (TH1)

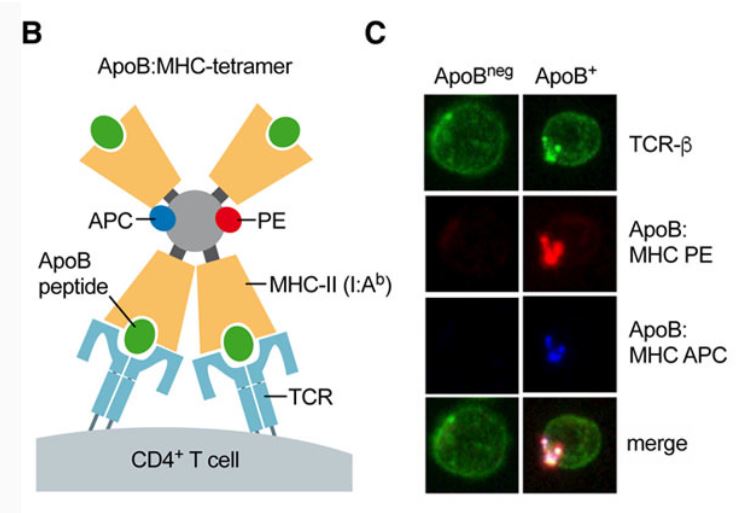
为了探讨自身反应性CD4+ T细胞在动脉粥样硬化中的作用,研究人员采用一种新型的主要组织相容性复合体II四聚体在单细胞水平上追踪T细胞对小鼠自身肽apo B978-993 (apoB+)的反应。
结果发现,apoB+ T细胞在健康小鼠淋巴结中构建了一种寡克隆群体,表现为Treg样转录组,仅21%的apoB+ T细胞表达Treg转录因子FoxP3蛋白。在单细胞RNA测序中,apoB+ T细胞形成了几个带有混合TH特征的集群,提示与TH1、2型T辅助细胞(TH2)、17型T辅助细胞(TH17)和滤泡性辅助T细胞的促炎和抗炎转录本有多谱系表型重叠。
原始出处:
Dennis Wolf, et al. Pathogenic Autoimmunity in Atherosclerosis Evolves From Initially Protective Apolipoprotein B100–Reactive CD4+ T-Regulatory Cells. Circulation. 2020;142:1279–1293. https://doi.org/10.1161/CIRCULATIONAHA.119.042863
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#致病性#
46
#粥样硬化#
38
#CD4#
31
学习!
102