Blood:霍奇金淋巴瘤肿瘤微环境中,CD4+效应T细胞耗竭、调节T细胞富集
2018-06-08 MedSci MedSci原创
中心点:新确诊的原发性cHLs伴随CD4+Th1极化调节T细胞和分化的效应T细胞增多。原发性cHLs表现出两种主要的免疫抑制互补——PD-1+Th1效应细胞耗竭和PD-1-Th1调节T细胞活化。摘要:经典型霍奇金淋巴瘤(cHL)患者抗肿瘤免疫反应失效。霍奇金RS(HRS)细胞有多种逃脱免疫细胞的机制,包括9p24.1/CD274(PD-L1)/PDCD1LG2(PD-L2)遗传变异、PD-1配体过
新确诊的原发性cHLs伴随CD4+Th1极化调节T细胞和分化的效应T细胞增多。
原发性cHLs表现出两种主要的免疫抑制互补——PD-1+Th1效应细胞耗竭和PD-1-Th1调节T细胞活化。
摘要:
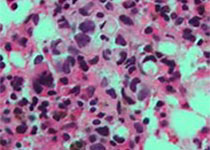
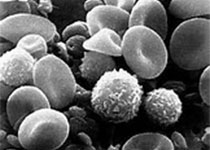
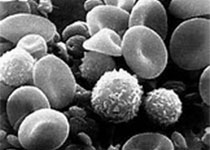
经典型霍奇金淋巴瘤(cHL)患者抗肿瘤免疫反应失效。霍奇金RS(HRS)细胞有多种逃脱免疫细胞的机制,包括9p24.1/CD274(PD-L1)/PDCD1LG2(PD-L2)遗传变异、PD-1配体过表达、相关T细胞耗竭以及异常抗体呈现的额外的结构基础。临床上成功封闭cHL患者的PD-1提示肿瘤微环境(TME)包括可逆性耗竭T效应细胞(Teff)。但是,在HRS细胞β2M/I型MHC丢失的患者中可观察到持续反应,提示非-CD8+T细胞可能也介导PD-1封闭效应。上述发现强调需对cHL肿瘤微环境进行详细分析。
研究人员同时评估来源于诊断性cHL活检和对照反应淋巴结/扁桃体(RLNT)样本的细胞悬液。免疫细胞亚型的精确表型显示cHLs和RLNTs之间存在显着差异。cHL的肿瘤微环境中CD4+T细胞富集伴随HRS细胞I型MHC表达频繁丧失。
研究人员还发现,在cHLs中,Th1极化的T辅助细胞和调节T细胞同时扩增。cHL Th1调节T细胞少量表达或不表达PD-1,而Th1辅助T细胞为PD-1+。
PD-1表达差异、Th1极化的CD4+调节T细胞的可能功能和T辅助细胞耗竭或许是cHL免疫抑制的互补机制。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#T细胞耗竭#
46
#CD4#
37
#调节T细胞#
0
#CD4+#
35
学习了谢谢分享
85
学习了.长知识
99