FDA核准Rapid Medical的世界首条可操控神经血管导丝
2020-12-24 国际文传 国际文传
专注于开发一流响应式、可调节神经血管器械的公司Rapid Medical宣布,FDA已核准DRIVEWIRE,这种新颖的导丝具有可操控的远端末梢,可轻松处理复杂的解剖学转向。
专注于开发一流响应式、可调节神经血管器械的公司Rapid Medical宣布,FDA已核准DRIVEWIRE,这种新颖的导丝具有可操控的远端末梢,可轻松处理复杂的解剖学转向。该器械在美国境外被称为Columbus。
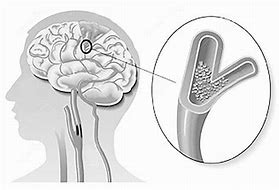
借助DRIVEWIRE,医生可在导丝末梢位于血管腔内时控制其方向和形态,精准探查神经和周围血管。通过这种血管内操控,可进入难以到达的解剖部位,提高医生以侵入性较小的介入方式治疗血管疾病的能力。
导丝是治疗缺血性和出血性卒中等血管内疾病的关键组件。目前,医生不能直接控制导丝末梢,在到达所需部位之前常多次移除导丝以重塑其形态。DRIVEWIRE是首款具有可操控远端的神经血管导丝,能按需改变路径和形态以实现更精准的探查。这使医生能够选择最为高效安全的路径来到达解剖部位。
纽约州纽约市纽约大学朗格尼医学中心的神经外科医生Erez Nossek医生评论道:“DRIVEWIRE的开发是一次令人振奋的合作。现在我能通过改变导丝末梢在血管内的形态来轻松探查复杂的解剖结构,而现有的各种神经血管导丝均无法做到这一点。我希望这种首创的技术能造福具有挑战性解剖结构的患者,为他们提供更多的介入治疗选择。”
关于Rapid Medical
Rapid Medical正在开发改变神经血管治疗格局的器械。Rapid Medical的器械运用新颖的制造技术,是首批可远程调节的工具,可提供更好的控制以实现更好的手术结果。TIGERTRIEVER™、COMANECI™和COLUMBUS™均获得CE认证,可在欧洲使用。COMANECI和DRIVEWIRE™同时获得FDA核准。欲了解更多信息,请访问www.rapid-medical.com。
原文阅读:http://www.businesswirechina.com/zh/news/45387.html
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIC#
34
#导丝#
42
#Medical#
23
#Med#
0
好文章!
56
🤙🤙🤙🤙🤙🤙
50