Clinica Chimica Acta:循环生长分化因子-15、kruppel样因子4和生长阻滞剂特异性6与冠心病的关系
2019-10-17 gladiator MedSci原创
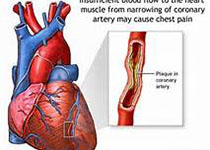
目前用于急性胸痛患者的评估工具要么是创伤性的(冠状动脉造影),要么可靠性较差(心肌肌钙蛋白浓度的测量)。
目前用于急性胸痛患者的评估工具要么是创伤性的(冠状动脉造影),要么可靠性较差(心肌肌钙蛋白浓度的测量)。我们研究了新的心血管应激标志物、血清生长分化因子-15 (GDF-15)、kruppel样因子4 (KLF4)和生长抑制因子特异性6 (gas6)是否可能成为冠心病(CAD)的有用生物标志物。
根据冠状动脉造影,本研究共纳入350名男性患者,包括198名冠心病患者和152名对照组。采用酶联免疫吸附试剂盒检测GDF-15、KLF4和gas6浓度。采用多因素logistic回归和多因素线性回归分析GDF-15、KLF4和gas6与冠心病风险或冠心病严重程度之间的关系。
血清GDF-15,KLF4和GAS6浓度男性患者显著高于CAD比对照组(P <0.05),且它们与冠状血管介入(P <0.05)显著相关。调整混杂因素后,我们发现,循环GDF-15浓度保持正与CAD的存在(比值比[OR]每1标准差[SD]增加,3.182; 95%置信区间[CI] 1.586至6.382 ; P =
0.001),象KLF4浓度(OR每1-SD增加,13.05; 95%CI 2.940到57.921,P = 0.001)。此外,循环GDF-15浓度呈正Gensini评分(每1-SD增加估计SD改变,22.091; 95%CI 9.147到35.035,P = 0.001)相关联,因为是KLF4浓度(每1-估计SD变化SD增加,27.996; 95%CI 10.082
45.910到,P = 0.002)。 相比之下,Gas6与CAD或Gensini评分无关。
在本病例对照研究中,循环GDF-15和KLF4浓度升高与冠心病的存在和严重程度显著相关。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#生长分化因子-15#
24
#CTA#
26
#阻滞剂#
41
#特异性#
33
#PE#
25
#PEL#
38