AJNR:CEA后再狭窄的颈动脉血管壁MR特征有助于制订下一步治疗决策
2022-04-26 杨中华 “脑血管病及重症文献导读”公众号
颈动脉内膜切除术(carotid endarterectomy,CEA)能够降低卒中的风险,是严重狭窄的标准治疗方案,术后再狭窄占1-36%,是其长期疗效的重要决定因素。组织学研究表明,复发性颈动脉狭
颈动脉内膜切除术(carotid endarterectomy,CEA)能够降低卒中的风险,是严重狭窄的标准治疗方案,术后再狭窄占1-36%,是其长期疗效的重要决定因素。组织学研究表明,复发性颈动脉狭窄主要是由于术后早期(2年内)的肌内膜增生(myointimal hyperplasia,MH)和术后复发性动脉粥样硬化所致。虽然MH在早期更常见,但其时间跨度很宽,在时间上与复发性动脉粥样硬化有明显的重叠。复发性斑块和MH具有不同的病理成分,可能有助于指导治疗策略。沿着血管壁的MH,其成分变化不大,主要由平滑肌细胞和胶原组成。这些MH病变不容易发生溃疡或发生出血和栓塞,因此针对MH再次进行CEA治疗的获益比治疗复发性斑块的获益更小。如果这些患者无症状且无严重狭窄,则无创性监测可能更适合这些患者。相反,斑块复发特别是具有高风险特征的斑块(脂质核心或斑块内出血[intraplaque hemorrhage,IPH]),更容易引起栓塞和脑血管事件,这些患者需要手术治疗。因此,再次手术之前对颈动脉再狭窄的特征进行评估以确定最佳治疗方案是必要的。
图1.从CEA后正常形态发展到MH。CEA手术后2个月,TOF-MRA(A)显示预期的血管形态。ICA近端同一部位(A中的直线)的增强前(B)和增强后(C)血管壁MRI(vessel wall MR imaging,VWMRI)显示血管壁增强,但ICA近端没有血管壁异常增厚(长箭头)。CEA10个月后TOF-MRA(D)显示管腔狭窄。在相同部位(D中的直线)的增强前(E)和增强后(F)VWMRIs显示血管壁环形增厚,伴有轻度不均匀强化,符合MH的特征(长箭头)。B,C,E和F中的短箭头表示颈外动脉:
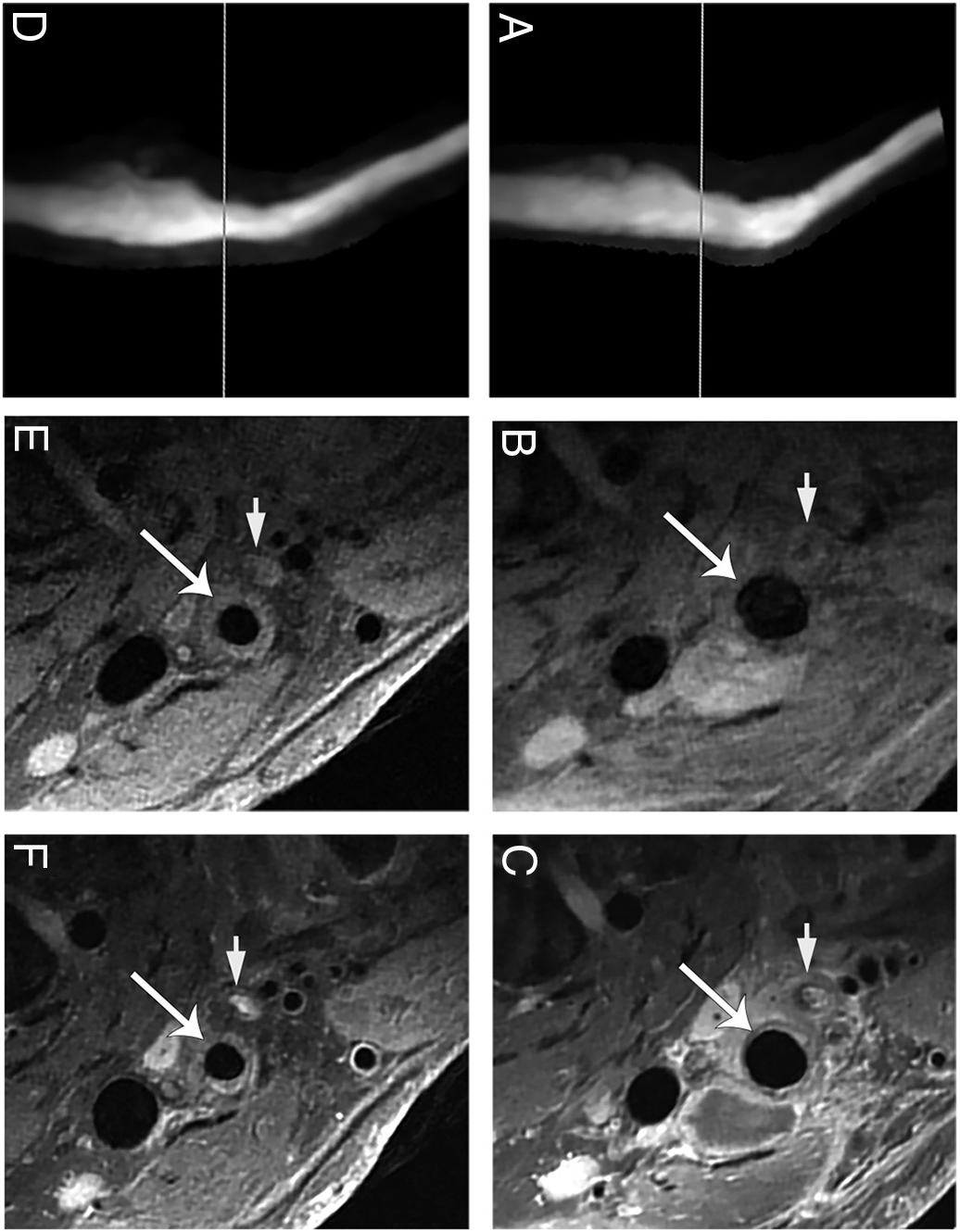
图2.MH示例。TOF-MRA(A)显示CEA后再狭窄,从颈动脉分叉处近端延伸至远端。ICA近端(A中的直线)增强前VWMRI(B)显示血管壁同心均匀增厚(长箭头),提示MH。增强后VWMRI(C)显示病变强化(长箭头)。B和C中的短箭头表示颈外动脉:
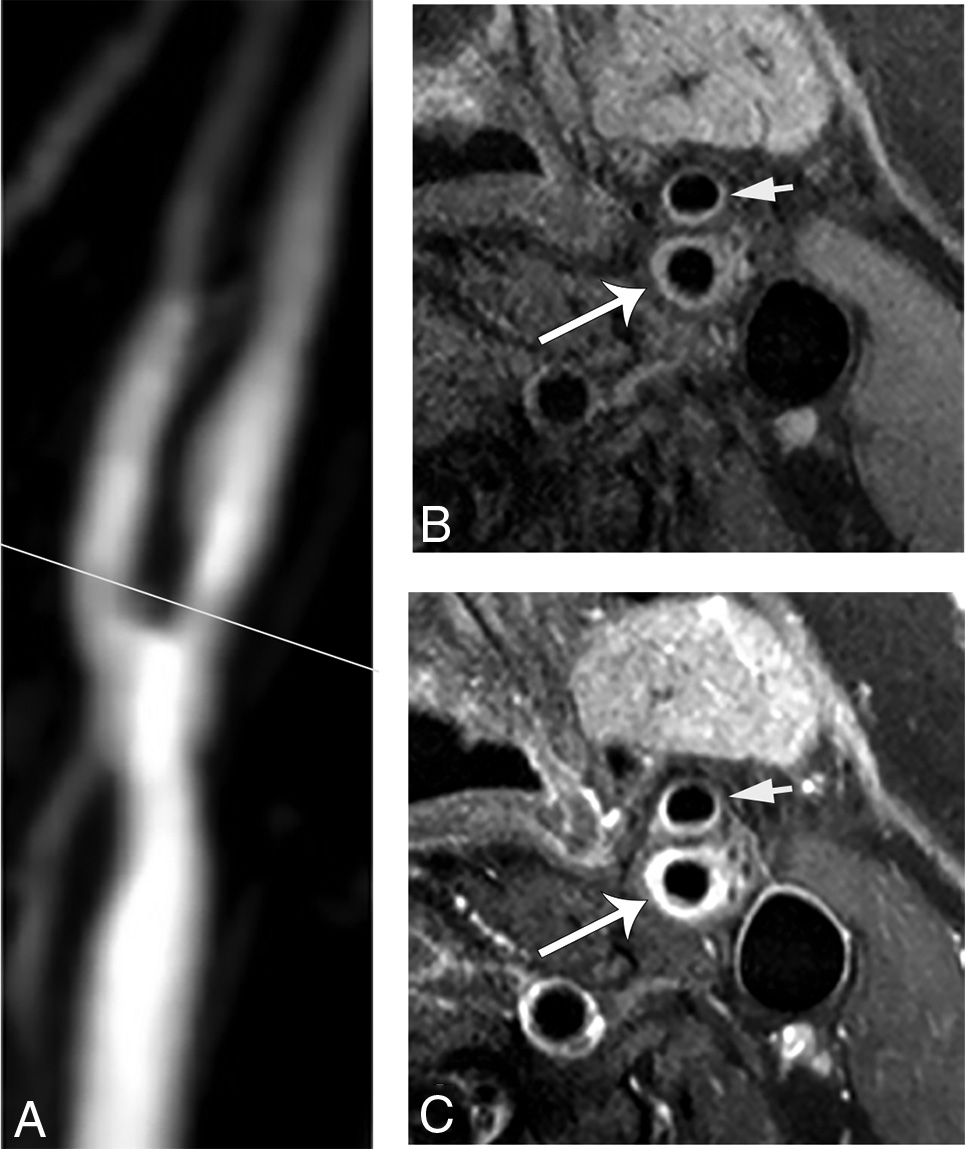
图3.复发斑块示例。TOF-MRA(A)显示颈动脉球部高度再狭窄。白线表示VWMRI的位置。增强前(B,左图)和增强后(B,右图)VWMR显示血管壁增厚,偏心强化,伴溃疡(星号),提示复发性斑块。MOVAT染色的相应标本切片(C)证实了复发性斑块。星号表示溃疡。B和C中的箭头代表管腔:

原始出处:
W Yang, et al. Characterization of Restenosis following Carotid Endarterectomy Using Contrast-Enhanced Vessel Wall MR Imaging. AJNR Am J Neuroradiol. 2022 Mar;43(3):422-428. doi: 10.3174/ajnr.A7423. Epub 2022 Feb 17.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#下一步#
45
#动脉血#
40
#颈动脉#
49
#血管壁#
45
#再狭窄#
42
#CEA#
38
#治疗决策#
40
#决策#
39