Oncotarget:研究揭示NONHSAT062994抑制结直肠癌发生发展的机制
2017-10-21 MedSci MedSci原创
长非编码RNAs(lncRNAs)的异常表达与癌症的发生发展有关。然而,NONHSAT062994调控结肠直肠癌(CRC)的临床意义和机制目前尚不清楚。本研究中,研究发现NONHSAT062994在人类CRC组织和细胞系中明显下调。此外,其表达与CRC患者的肿瘤大小和总生存期(OS)时间呈负相关。体外和体内研究显示,CRC细胞中NONHSAT062994的过表达和敲低分别可抑制和增强CRC细胞的生
长非编码RNAs(lncRNAs)的异常表达与癌症的发生发展有关。然而,NONHSAT062994调控结肠直肠癌(CRC)的临床意义和机制目前尚不清楚。
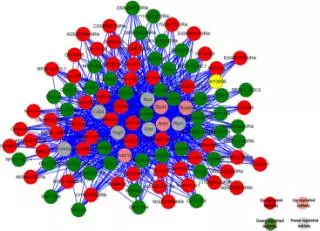
本研究中,研究发现NONHSAT062994在人类CRC组织和细胞系中明显下调。此外,其表达与CRC患者的肿瘤大小和总生存期(OS)时间呈负相关。体外和体内研究显示,CRC细胞中NONHSAT062994的过表达和敲低分别可抑制和增强CRC细胞的生长。具体来说,NONHSAT062994可作为肿瘤抑制剂,通过失活Akt信号传导来抑制CRC细胞的生长。值得注意的是,NONHSAT062994的表达状态与临床CRC样品中Akt下游靶标c-Myc和Cyclin D1呈负相关。
总之,目前的研究结果表明,NONHSAT062994通过调节Akt信号通路在CRC的发生发展中发挥关键作用,并确定了CRC的潜在预后生物标志物或治疗靶标。
原始出处:
Xiao-Shun He, Ling-Chuan Guo, et al., The long non-coding RNA NONHSAT062994 inhibits colorectal cancer by inactivating Akt signaling. Oncotarget. 2017 Sep 15; 8(40): 68696–68706. Published online 2017 Aug 2. doi: 10.18632/oncotarget.19827
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发生发展#
53
#target#
40
#结直肠#
35
#NHS#
40
学习了.谢谢
61
不错的文章值得一读
74