罗氏Actemra/RoActemra治疗巨细胞动脉炎维持无激素缓解(TFR)
2016-06-12 佚名 生物谷
瑞士制药巨头罗氏(Roche)近日公布了抗炎药Actemra/RoActemra(tocilizumab)治疗巨细胞动脉炎(GCA)的一项III期临床研究(GiACTA)的积极数据。数据显示,在新诊和复发GCA患者中,与6个月或12个月类固醇方案相比,Actemra/RoActemra在最初的6个月联合类固醇(糖皮质激素)治疗,能够更有效地维持缓解持续一年。该研究中,在数据分析时未发现新的安全性
瑞士制药巨头罗氏(Roche)近日公布了抗炎药Actemra/RoActemra(tocilizumab)治疗巨细胞动脉炎(GCA)的一项III期临床研究(GiACTA)的积极数据。数据显示,在新诊和复发GCA患者中,与6个月或12个月类固醇方案相比,Actemra/RoActemra在最初的6个月联合类固醇(糖皮质激素)治疗,能够更有效地维持缓解持续一年。该研究中,在数据分析时未发现新的安全性信号。该研究的详细数据将提交至未来召开的科学会议。
GiACTA(NCT01791153)研究是一项全球性、随机、双盲、安慰剂对照III期研究,评估了Actemra/RoActemra作为GCA的一种新型治疗方案的疗效和安全性。该研究是迄今为止在GCA群体中开展的最大临床研究,达到了主要终点和全部关键次要终点。数据显示,Actemra能够帮助GCA患者维持无类固醇缓解(steroid-free remission)。
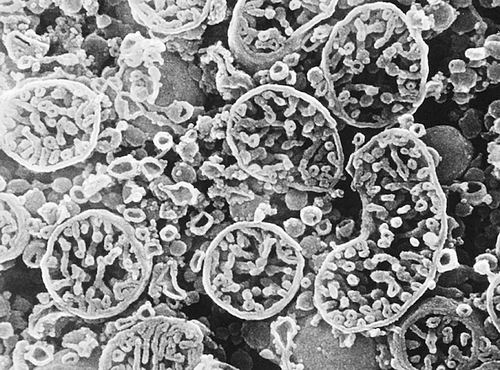
巨细胞动脉炎(GCA)是一种严重的动脉炎症疾病,常见于头部,但也见于主动脉及其分支。炎症可导致持续性的严重的头痛、头皮压痛、下巴和手臂疼痛。GCA很难诊断,如果不及时治疗,可能导致失明、中风和动脉瘤。据估计,视觉问题发生于大约30%的GCA患者,大约15%的患者会发生永久性视力丧失。
GCA临床治疗在过去50多年无新的治疗方法。目前,GCA的主要治疗方案是长期的高剂量类固醇治疗,但可能引起严重的副作用。如果获批,Actemra/RoActemra将为GCA患者提供取代长期类固醇治疗的一个重要新选择。
据估计,高达80%的GCA患者接受长期类固醇治疗会经历严重副作用,包括白内障、糖尿病、骨折和高血压。在临床上,降低类固醇使用是GCA患者临床治疗的一个重要目标。
ACTEMRA/RoACTEMRA是首个可通过静脉输注(IV)和皮下注射(SC)2种方式给药的人源化白细胞介素6受体拮抗剂单克隆抗体,已获全球多个国家批准用于中度至重度活动性类风湿性关节炎(RA)成人患者的治疗。
ACTEMRA/RoACTEMRA可单独用药或与甲氨蝶呤(MTX)联合用药,用于对其他抗风湿药物不耐受或无响应的成人患者。ACTEMRA/RoACTEMRA静脉注射配方(IV)已获全球主要市场批准用于2岁及以上幼年特发性关节炎(pJIA)或全身性幼年特发性关节炎(sJIA)患者的治疗。在欧洲,ACTEMRA/RoACTEMRA也已获批用于既往未使用甲氨蝶呤(MTX)治疗的严重活动性进展性类风湿性关节炎(早期RA)成人患者的治疗。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#EMR#
24
#动脉炎#
24
#巨细胞#
38
#Actemra#
32
#RoActemra#
30
#MRA#
32