Lancet:重磅:III期研究显示肝癌治疗新药仑伐替尼有望成为一线治疗晚期肝癌标准
2018-02-12 肿瘤资讯编辑部 肿瘤资讯
肝癌是中国高发肿瘤,晚期肝癌的药物治疗研究中国一直处于世界前列。2018春节将至之际,中国肝癌研究者参与的国际、多中心临床研究结果在线发表在国际顶级医学杂志《柳叶刀》主刊上。由于该研究对肝癌的临床意义巨大,《柳叶刀》也特意为该研究配了评论性文章。
肝癌是中国高发肿瘤,晚期肝癌的药物治疗研究中国一直处于世界前列。2018春节将至之际,中国肝癌研究者参与的国际、多中心临床研究结果在线发表在国际顶级医学杂志《柳叶刀》主刊上。由于该研究对肝癌的临床意义巨大,《柳叶刀》也特意为该研究配了评论性文章。秦叔逵教授等中国学者在该研究中共入组患者近300例,贡献巨大。该研究中的亚洲患者的亚组分析数据在去年的CSCO年会上由秦叔逵教授公布。
研究背景
在II期研究中多靶点抗VEGF的小分子抑制剂仑伐替尼(Lenvatinib)在肝癌中显示出临床活性。本III期研究的目的是比较仑伐替尼 vs 索拉非尼作为不可切除肝癌患者一线治疗的总生存期的随机对照研究。
研究方法
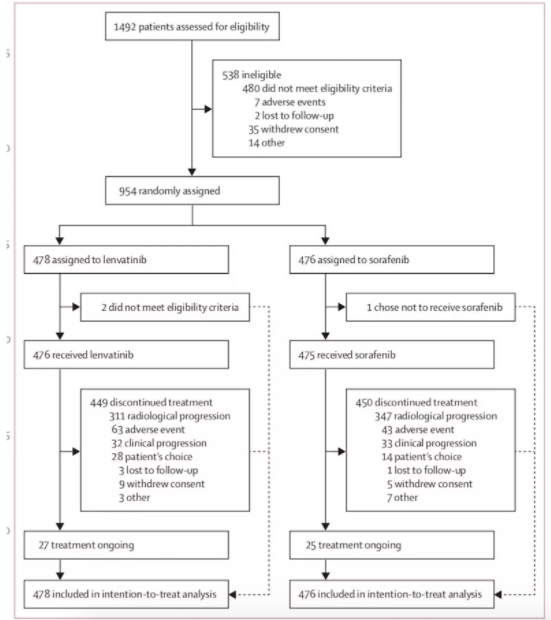
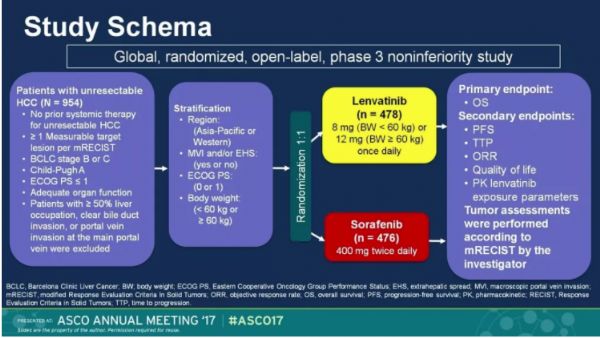
这是一项开放的、多中心、III期非劣效研究,入组患者为既往未接受过治疗的、不可切除性晚期肝细胞癌患者,研究中心来自亚太、欧洲和北美的20多个国家的154个地区。患者随机按1:1分配,ECOG评分和体重情况作为分层因素。
口服仑伐替尼(体重≥60 kg者,12mg/天;体重<60 kg者,8 mg /天)或索拉非尼400 mg,2次/天,每28天为一个周期。主要终点是总生存期(OS,从随机分组开始到任何原因导致死亡的时间)。只有接受治疗的患者才纳入安全性分析。非劣效边缘定为1.08。该试验已在ClinicalTrials.gov注册,编号为NCT01761266。
研究结果
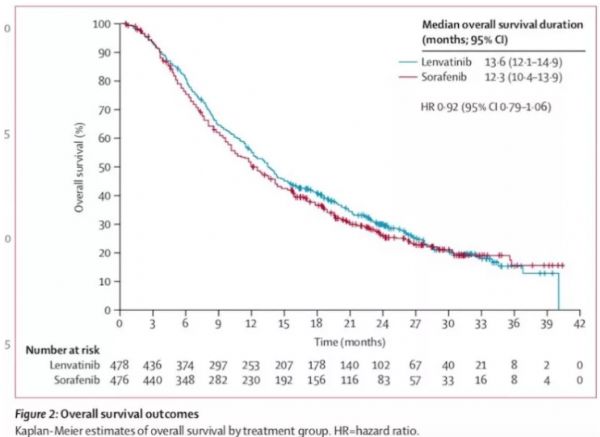
2013年3月1日至2015年7月30日,共招募了1492名患者。 954名符合条件的患者被随机分配到仑伐替尼(n = 478)或索拉非尼(n = 476)。 仑伐替尼中位生存期为13.6个月(95%CI 12.1〜14.9),与索拉非尼组相比无差异(12.3个月,10.4-13.39;HR=0.92,95%可信区间 0.79-1.06),符合非劣效性标准。 仑伐替尼最常见的任何级别的不良事件是高血压(201 [42%])、腹泻(184 [39%])、食欲下降(162 [34%])和体重减轻(147 [31%])。索拉非尼最常见的不良反应为肢端红肿症(249 [52%])、腹泻(220 [46%])、高血压(144 [30%])和食欲下降(127 [27%])。
结论 在未经治疗的晚期肝细胞癌中,仑伐替尼的总生存率并不逊色于索拉非尼。 仑伐替尼的安全性和耐受性与之前观察到的一致。
讨论
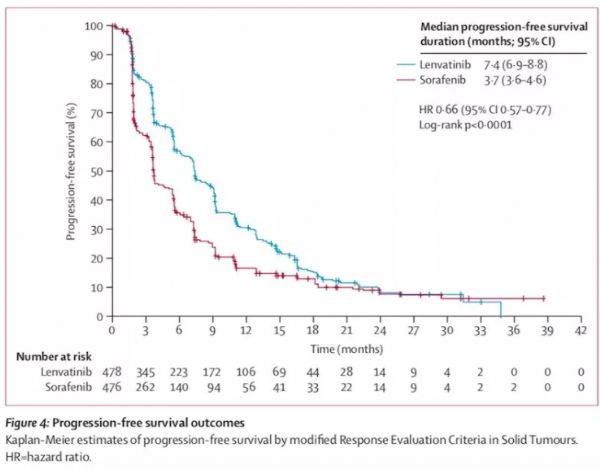
这是10年来第一个全球的III期临床研究,证明新药(仑伐替尼)和目前的标准治疗(索拉非尼)在总体生存上显示出非劣的治疗效果。同时该研究中仑伐替尼显示所有次要终点(包括:无进展生存期(PFS),进展时间和客观反应率ORR)在各个亚组,以及生活质量评估方面具有显着的临床意义改善。
该研究中接受索拉非尼治疗的患者的中位总生存时间比以前III期研究要长,其原因是索拉非尼治疗失败后接受后续治疗的比例很高。
总之,本研究显示,仑伐替尼与索拉非尼在总生存率方面的非劣效性,以及无进展生存期,进展时间和客观缓解率的具有统计学意义和临床意义的改善。在该研究中,仑伐替尼和索拉非尼的安全性程度与这些药物在肝细胞癌中已知的安全性相一致,没有发现新的安全性问题。
秦叔逵教授点评
秦叔逵教授介绍:仑伐替尼是VEGF受体1-3、纤维母细胞生长因子受体1-4、血小板衍生生长因子受体α、RET和KIT的小分子抑制剂。其III期临床研究REFLECT是一项全球、多中心、随机对照临床研究。该研究是与索拉非尼头对头比较的非劣效试验,入组不可切除的肝细胞肝癌(uHCC)患者954例,其中中国大陆和港台地区患者近300例。在主要终点方面,仑伐替尼组OS较索拉非尼组有延长趋势(mOS:13.6个月vs. 12.3个月);在次要终点方面,仑伐替尼组的中位无进展生存时间(mPFS:7.4个月 vs. 3.7个月)、中位疾病进展时间(mTTP:8.9个月vs. 3.7个月)、客观有效率(ORR: 24% vs. 9%)则显著优于索拉非尼组。
秦教授指出:中国晚期肝癌研究走过很多弯路,该研究的成功不是偶然的,是在吸取了过去的许多经验教训的基础上获得的!在药物设计方面,仑伐替尼与索拉非尼都是抗血管生成剂,但仑伐替尼作用的靶点更集中、抑制作用更强;在试验的设计、管理、执行以及试验方案的把控方面,也做得也非常好,这也是能取得成功的重要因素。
秦教授特别指出,该研究的成功对于亚洲尤其是中国肝癌患者意义重大。中国晚期肝癌的生存期较欧美国家更短,且此前唯一的靶向药物索拉非尼的临床研究显示,其对HBV相关肝癌的疗效不佳,而在中国,因HBV感染引起的肝癌占总病例的90%以上,因此,中国晚期肝癌患者面临的临床挑战更为严峻。可喜的是,在仑伐替尼 III期临床研究中,我们看到其对中国肝癌患者、HBV相关肝癌的有效性明显优于索拉非尼,提示仑伐替尼更适合中国肝癌患者。“这是非常值得我们期待的”。
原始出处:
Masatoshi Kudo, Richard S Finn, Shukui Qin, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. The Lancet. Feb 9, 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#III#
31
#III期研究#
33
#肝癌治疗#
33
#Lancet#
27
学习了
73
#重磅#
24
#III期#
39