J Clin Oncol:双打击淋巴瘤:一线强化化疗比自体移植更重要?
2017-05-15 任我行 肿瘤资讯
在传统的R-CHOP方案治疗的前提下,双打击淋巴瘤预后极差,既往的回顾性研究表明,强化化疗与自体移植似乎可以改善患者的预后,对于取得首次完全缓解的双打击淋巴瘤患者,两者的意义到底如何,来自美国的一项多中心、回顾性研究似乎给了我们答案。背景双打击淋巴瘤(double-hit lymphoma, DHL),是指伴有MYC基因重排与BCL2基因和/或BCL6基因重排的B细胞非霍奇金淋巴瘤,DHL呈高
在传统的R-CHOP方案治疗的前提下,双打击淋巴瘤预后极差,既往的回顾性研究表明,强化化疗与自体移植似乎可以改善患者的预后,对于取得首次完全缓解的双打击淋巴瘤患者,两者的意义到底如何,来自美国的一项多中心、回顾性研究似乎给了我们答案。
背景
双打击淋巴瘤(double-hit lymphoma, DHL),是指伴有MYC基因重排与BCL2基因和/或BCL6基因重排的B细胞非霍奇金淋巴瘤,DHL呈高度侵袭,预后极差,中位生存小于2年。 鉴于DHL的预后极差,有研究者试图通过提高一线化疗的强度来提高患者的预后。尽管早期的单中心研究未能得出一线高强度化疗使患者获益的结论,但是两项大型的回顾性研究提示,相对于R-CHOP方案,一线高强度化疗可以提高患者的无进展生存(PFS)但不是总生存(OS)。
另外一种提高一线化疗强度的方法是在DHL取得首次取得完全缓解后(CR1)进行自体干细胞移植(autoSCT)。鉴于DHL在复发之后预后极差,CR1之后进行autoSCT巩固显得十分重要。尽管autoSCT可以显着取得CR1的高度侵袭性非霍奇金淋巴瘤的PFS,但是,现有的两大回顾性的研究中并没有明确autoSCT是否能使取得CR1的患者获益(因为样本数较小,取得CR1的患者更少)。
在本研究中,通过多中心大样本研究,研究者分析了一线治疗与autoSCT对取得CR1的患者生存和复发的影响。
结果
研究纳入了来自美国19个中心的159位患者,在159例患者中,62例患者接受了autoSCT,97例患者没有接受autoSCT,与没有autoSCT的患者相比,接受autoSCT的患者更加年轻,骨髓累及更少,更多的患者具有惰性淋巴瘤的病史。
中位随访时间26.5个月时,3年的无复发生存(RFS)率和3年的总生存率分别为80%和87%。不接受autoSCT和接受autoSCT的患者的患者,在3年的RFS率(75% vs 89%; p = 0.12)和3年的OS率 (85% vs 91%; p = 0.74)没有显着差异(图一)。在非转化的139例患者中,不接受autoSCT(n=91)和接受autoSCT (n=48)在3年的RFS率(74% vs 88%, p = 0.15)和3年的OS率 (84% vs 91%, p = 0.68)方面相似。不接受autoSCT的患者与接受autoSCT患者相比,接受的中枢预防(57% vs 75%; p =0 .02)和强化的化疗更少 (72% v 87%; p =0 .03)。
然而,接受不同一线化疗方案的患者,3年的PFS率有显着差异,R-CHOP (n = 35),DA-EPOCH-R (n = 81),R-hyperCVAD (n = 32)和R-CODOX-M/IVAC (n=11)的患者的3年的PFS率分别为56%, 88%, 87%和 91%(p=0.003)(图二),但是四组患者的3年OS率没有显着差异(分别为77%,87%,90%,100%)。接受强化化疗的3组患者(DA-EPOCH-R,R-hyperCVAD和R-CODOX-M/IVAC)的3年的PFS率(p=0.90)和OS率(p=0.57)没有显着差别。接受强化化疗的3组患者总体的3年PFS率为88%,显着高于R-CHOP组(56%, p=0.002),3年的OS率有差异但无统计学意义(90% vs 77%, p=0.13)。
R-CHOP组在CR1时不接受autoSCT(n=27)的患者,其3年PFS和OS率分别为51%和75%,而对于接受autoSCT的患者(n=9),其3年PFS和OS率分别为75%和83%。而对于接受强化化疗处于CR1时不接受autoSCT的患者(n=70),3年的PFS和OS率分别为86%和89%,对于CR1接受autoSCT的患者(n=54),3年的RFS率和OS率分别为91%和92%。接受R-CHOP方案但不接受autoSCT的患者其3年的RFS率要显着低于接受强化化疗(有/无autoSCT)的患者,但3年的OS率无显着差异。
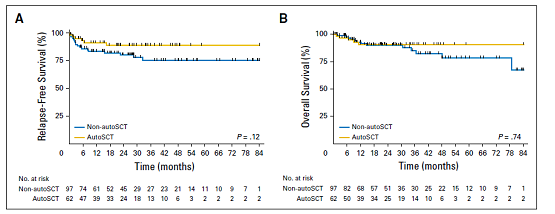
图一.接受autoSCT和不接受autoSCT的患者RFS和OS并无显着差异

图二.不同方案对于RFS和OS的影响
共有25例患者复发,复发后中位OS为8.6个月,不同的化疗方案以及是否接受autoSCT对于复发后的OS没有显着影响。在复发的25例患者中,共5例患者为中枢复发,其中3例患者在一线治疗中接受过中枢预防。
讨论
DHL预后极差,既往的研究表明,强化的一线免疫化疗可能可以提高DHL患者的预后。接受DA-EPOCH-R或HyperCVAD此类强化化疗方案的患者与接受R-CHOP,具有更高的首次完全缓解率(68% vs 40%)。DHL复发后的预后非常之差,3年的OS率仅为7%。复发之后再行autoSCT并不能很好的控制疾病,这使得在CR1时行autoSCT进行巩固预防复发变得非常重要。
在本研究中,在CR1时是否接受autoSCT对DHL的预后似乎并不造成影响。有趣的是,在都能取得首次完全缓解的前提下,接受R-CHOP方案的患者,其3年RFS率要显着低于接受强化化疗方案的患者。总体上来讲,接受R-CHOP方案但不接受autoSCT的患者预后最差,这对于临床实践的意义在于,对于接受R-CHOP方案后取得完全缓解的患者,autoSCT目前可能仍然是必要的。
结论
该研究表明,对于取得CR1的患者,仍无证据显示autoSCT可以提高患者的预后。R-CHOP方案在3年RFS率方面显着差于其他强化方案。鉴于目前缺乏前瞻性的研究数据,如果DHL情况许可,建议采用强化的化疗方案,若取得CR1,则不推荐进行autoSCT(一线为强化化疗)。
点评
DHL患者预后极差,使用R-CHOP方案CR率低,且即使取得CR,与强化化疗方案相比,其RFS率依然较低,对于CR1的患者,autoSCT的价值似乎不大,尤其是对于接受强化化疗方案的患者,所以,目前对于DHL,依然推荐使用强化化疗方案,对于CR1的患者,可以不使用autoSCT。
原始出处:
Landsburg DJ, Falkiewicz MK, Maly J, Chavez JC, et al. Outcomes of Patients With Double-Hit Lymphoma Who Achieve First Complete Remission. J Clin Oncol. 2017 May 5.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#双打击淋巴瘤#
32
#Oncol#
37
#自体移植#
29
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
73
涨知识了,标准的R_CHOP方案疗效却很差,谢谢分享。
84
学习了。
68
学习了,谢谢分享
73
感谢分享一下吧!!
84
学习
32