一文读懂|急性冠状动脉综合征的药物治疗
2018-04-06 佚名 嘉音
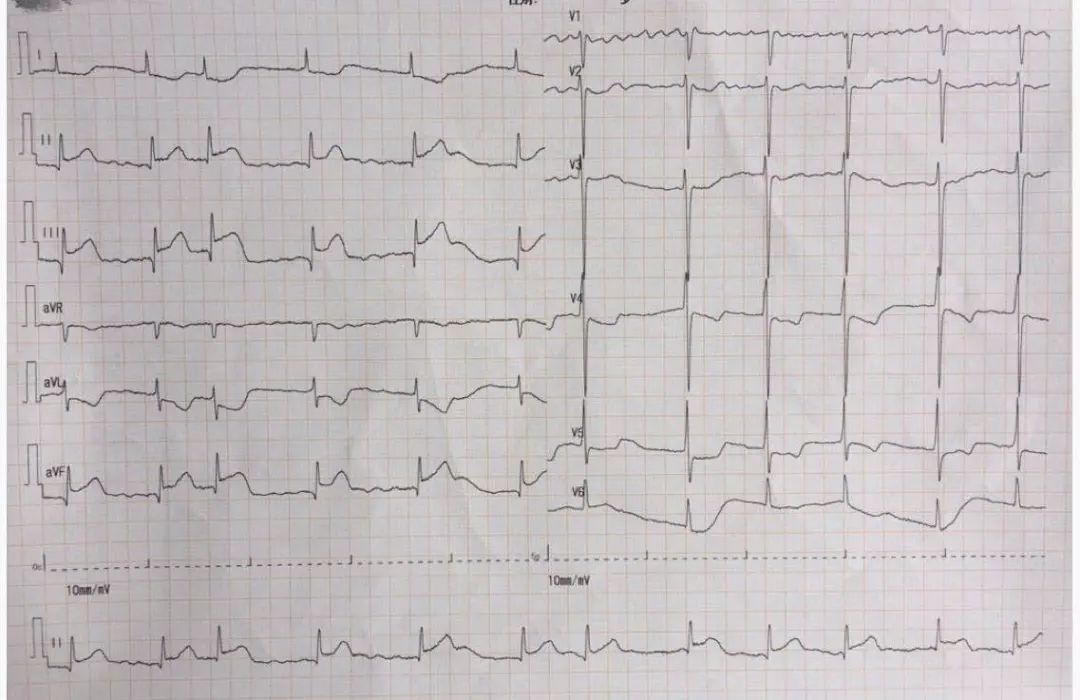
急性冠状动脉综合征(acute coronary syndrome,ACS)特指冠心病中急性发病的临床类型,主要涵盖以往分类中的Q波性急性心肌梗死(AMI)、非Q波性AMI和不稳定型心绞痛。由于上述三种临床类型都具有突然发病的特点,使人们自然联想到其发病可能具有共同的病理生理基础,即与斑块的不稳定有关,从而提出ACS概念。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#冠状动脉综合征#
35
学习一下谢谢
76
科普
75
学习学习学习
72
#综合征#
37
非常好.谢谢分享
59
一起学习学习
73
好文献.学习了
23
学习一下谢谢
31
学习了.谢谢分享.
25