Oncologist:许建民教授发现CERR得分能良好评估结直肠癌肝转移手术后复发状况
2020-05-16 MedSci MedSci原创
目前来说,手术切除在结肠癌肝转移治疗中具有最重要的里程碑意义,5年生存能够达到50%以上。结直肠肝转移手术切除的难点:①同时性肝转移是同时切除还是分阶段切除?现有研究支持具有高危因素的患者分阶段切除。
目前来说,手术切除在结肠癌肝转移治疗中具有最重要的里程碑意义,5年生存能够达到50%以上。结直肠肝转移手术切除的难点:①同时性肝转移是同时切除还是分阶段切除?现有研究支持具有高危因素的患者分阶段切除。②手术选择解剖性的肝脏切除还是非解剖局部切除。我们团队研究表明解剖性肝脏切除来意义不大,支持尽量保留肝脏实质的局部切除。
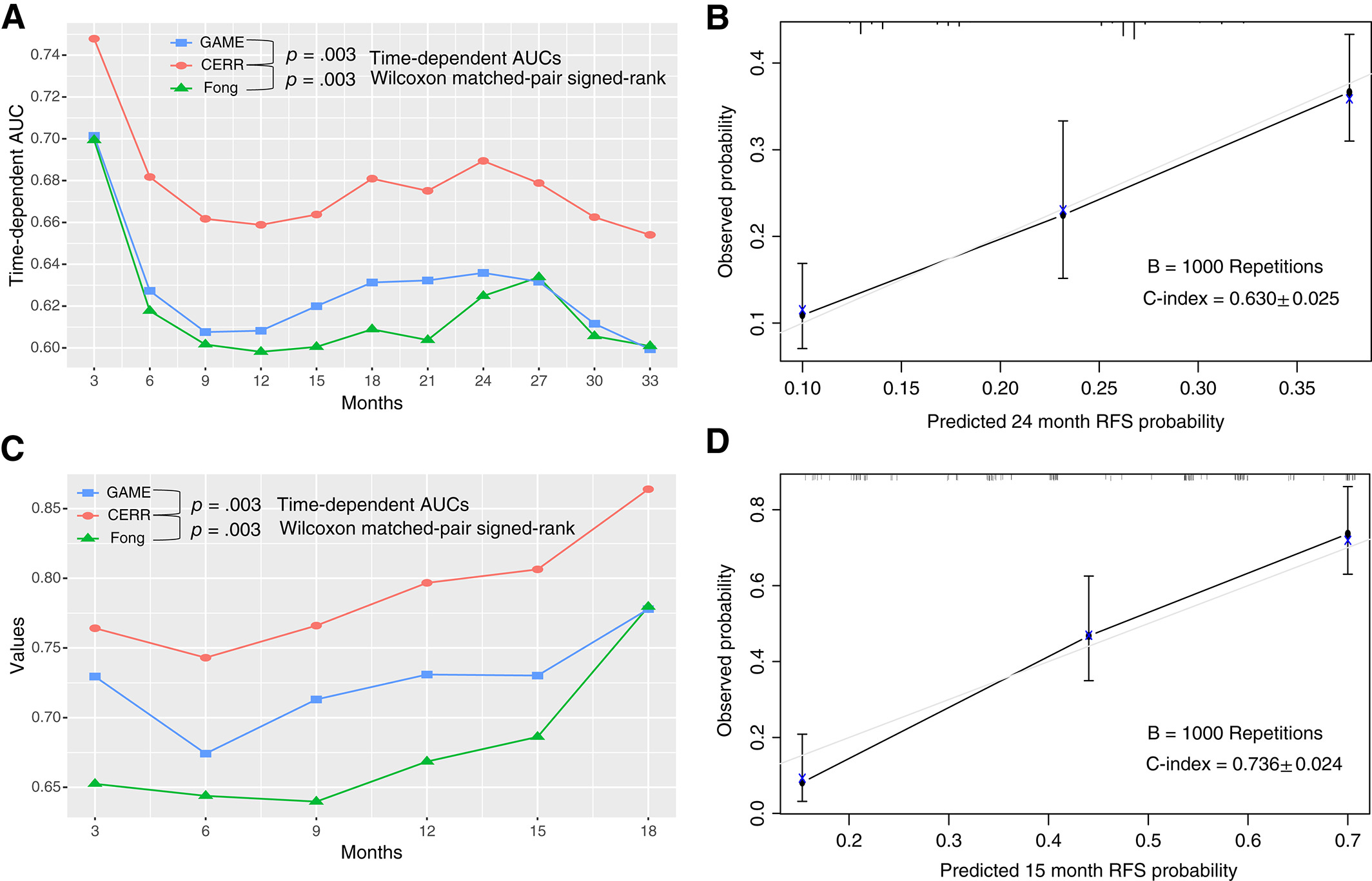
许建民教授团队分析了2010年6月至2018年1月间复旦大学附属中山医院因CRLM接受治疗性肝切除的787例成人患者的数据,以肿瘤无复发生存率(RFS)为其主要预后指标。通过几何算法,以CRLM大小、CRLM数目和单叶/双叶转移为参数,建立改良TBS(mTBS),结果显示,mTBS模型预测RFS优于TBS模型((33个月时AUC:0.62 vs. 0.54,P=0.002)。
进一步,将mTBS与其它4个因素联合作为术前预测因素,建立CERR评分,该评分纳入5个预测RFS的术前因素:①KRAS/NRAS/BRAF突变(1分),②原发性结节阳性(1分),③肝外疾病(1分),④CEA水平>200 ng/ml或CA19~9>200 U/ml(1分),⑤mTBS介于5~11(1分),12~12之间(2分)。
根据CERR评分将接受CRLM肝切除术的患者分为:高危组(CERR评分≥4分)3年RFS为9.77%;中危组(CERR评分2~3分)3年RFS为21.96%;低危组(CERR评分0~1分)3年RFS为39.90%。
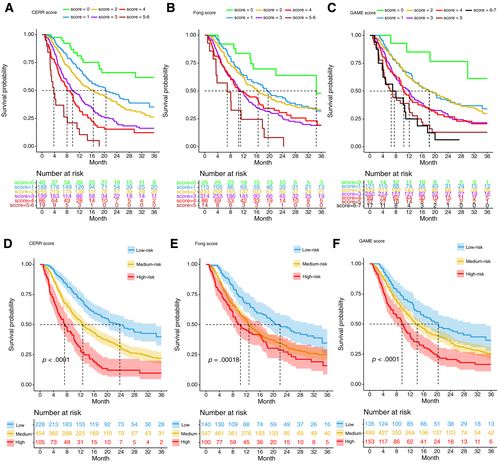
Bootstrap验证表明CERR评分的判别能力明显优于Fong’s临床风险评分和遗传形态学评价(GAME)评分。改良TBS可予以推广,CERR评分是一个强有力的预测工具,可以帮助制定最佳的临床决策。
风险评估是综合了结肠肝转移临床危险因素以及基因危险因素,比单纯CS评分更精准,更有效果。其疗效和指导意义更具临床价值。
在线应用mTBS模型:结直肠癌肝转移时肿瘤负荷得分(mTBS)
在线使用CERR模型:结直肠癌肝转移时复发风险综合评估得分(CERR Score)
许剑民教授
现任复旦大学附属中山医院结直肠外科主任。
卫生部大肠癌早诊早治专家组成员,卫生部《结直肠癌诊断和治疗标准》和《结直肠癌诊断和治疗规范》制定专家组成员,中国抗癌协会大肠癌专业委员以及大肠癌肝转移学组和遗传性大肠癌学组委员,国家自然基金和上海市科委基金评审专家,上海市疾病控制中心大肠癌中心组成员。《中华胃肠外科杂志》、《中国癌症杂志》、《肿瘤研究与临床杂志》和《消化肿瘤杂志》编委。《中华外科杂志》和《中国临床杂志》特约评审专家。
原始出处:
Chen Y, Chang W, Ren L, Chen J, Tang W, Liu T, Jian M, Liu Y, Wei Y, Xu J. Comprehensive Evaluation of Relapse Risk (CERR) Score for Colorectal Liver Metastases: Development and Validation.Oncologist. 2020 Mar 17. doi: 10.1634/theoncologist.2019-0797
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Oncol#
22
#术后复发#
0
#ERR#
37
#肝转移#
0
#结直肠#
46
#GIST#
37
可以在线使用,谢谢
4
谢谢梅斯分享这么多精彩信息
51