JAHA:西藏人群代谢危险因素与左室舒张功能的相关性研究
2019-03-15 不详 MedSci原创
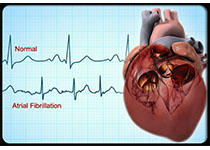
在高海拔和低氧环境下生活的人中,关于代谢危险因素聚类的左心室舒张功能障碍(LVDD)风险的数据尚缺乏。本研究的目的旨在中国西藏人群中探究代谢危险因素与LVDD的相关性。本研究纳入了1963名西藏人群,平均年龄51.51岁,男性占41.11%。其中LVDD的发病率为34.39%,1个危险因素、2个危险因素和3-5个危险因素的LVDD的风险比分别为1.45 (0.96–2.17), 2.68 (1.8
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#舒张功能#
42
#相关性#
38
#AHA#
37
好
64