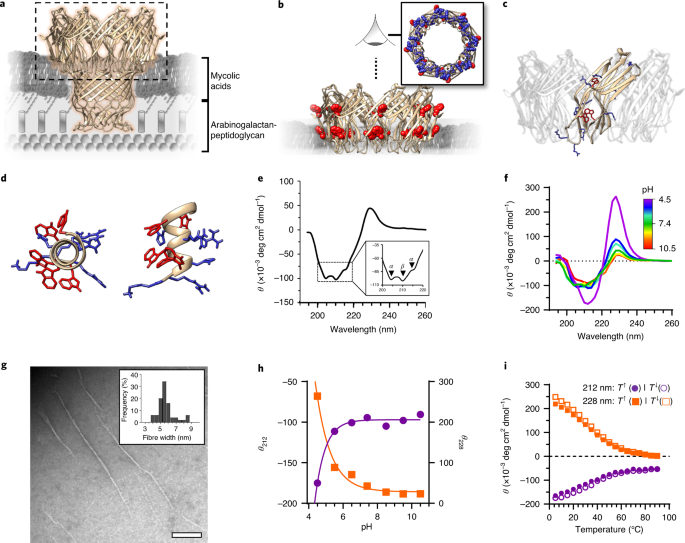
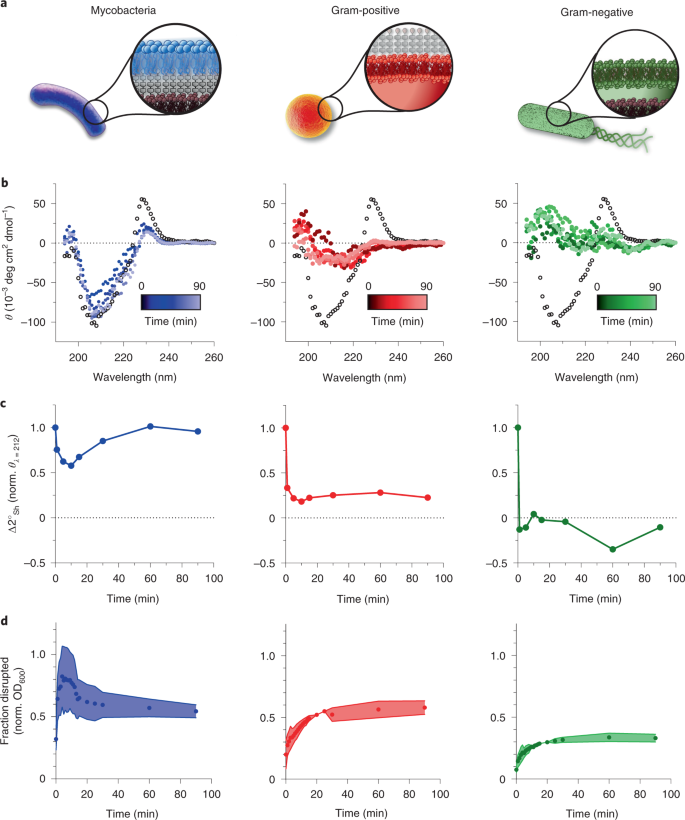
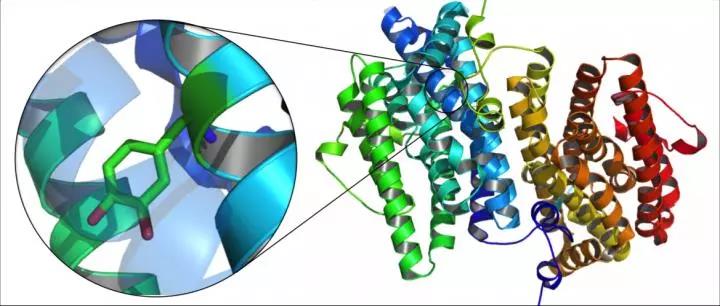
NAT BME:通过膜蛋白仿生从头构建病原体特异性抗菌剂
2021-01-30 MedSci原创 MedSci原创
小分子抗生素是目前我们对抗细菌感染的最好武器。它们的过度使用导致了多药耐药性的广泛出现。引起耐药性的一个未被充分认识但很重要的因素是人类微生物组。反复使用抗生素促进了过度暴露的共生菌群中耐药基因的积累
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
0
#特异性#
22
#膜蛋白#
33
#抗菌#
35
#病原体#
39