Sci Rep:生男生女大不同,高龄孕妇男性后代心血管疾病风险明显增高!
2019-12-02 Paris 转化医学网
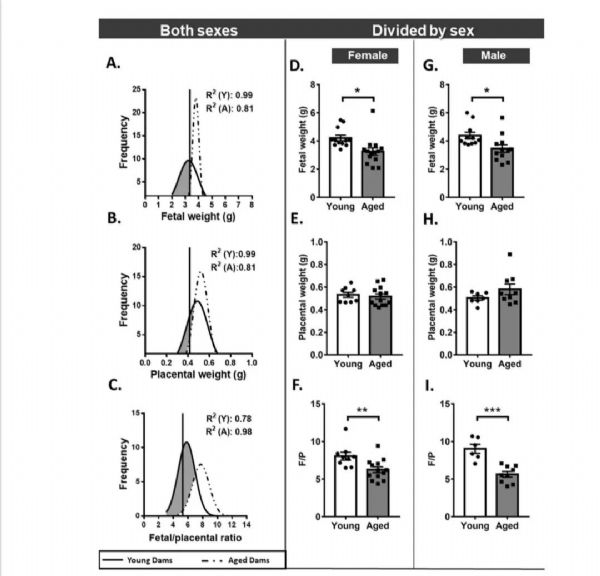
前段时间,67岁高龄孕妇产子的消息席卷全国。在二胎开放的当今,高龄孕妇(我国将年龄大于35岁的孕妇定义为高龄孕妇)愈发普遍,但其实,35岁以上的高龄产妇妊娠风险值呈明显上升趋势,出现难产、胎儿发育迟缓、先天性畸形儿以及孕产妇、胎儿死亡的几率要远远大于年轻产妇。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高龄#
44
#疾病风险#
41
#血管疾病#
33
#增高#
26
#增高#
30