Lancet:氨甲环酸早期短疗程治疗不能改善蛛网膜下腔出血患者的中短期预后
2020-12-22 MedSci原创 MedSci原创
目前已证明,动脉瘤性蛛网膜下腔出血患者采用氨甲环酸短期抗纤溶治疗可降低再出血的风险。但是,这种治疗是否可以改善临床预后尚不清楚。本研究旨在调查氨甲环酸超早期短疗程治疗是否可以改善6个月内的临床预后。
目前已证明,动脉瘤性蛛网膜下腔出血患者采用氨甲环酸短期抗纤溶治疗可降低再出血的风险。但是,这种治疗是否可以改善临床预后尚不清楚。本研究旨在调查氨甲环酸超早期短疗程治疗是否可以改善6个月内的临床预后。
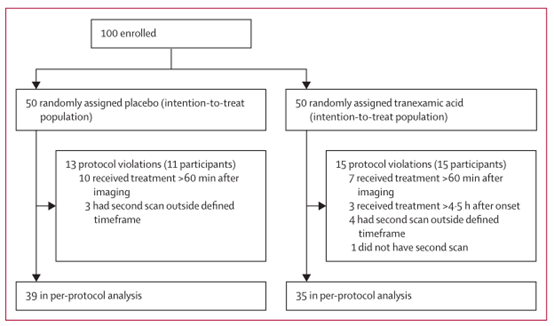
本研究是一项多中心、前瞻性、随机、对照、开放标签的临床试验,招募CT证实的自发性蛛网膜下腔出血成年患者,随机分组接受氨甲环酸+常规护理(氨甲环酸组)或仅常规护理(对照组)。氨甲环酸用药方法:一经确诊后即刻开始使用,1g推注,后1g/8h静滴维持,用满24h或开始动脉瘤治疗时停药。主要预后指标是6个月时的临床结局。
2013年7月24日-2019年7月29日,共招募了955位患者,其中480位被分至氨甲环酸组,475位被分至对照组。在意向治疗分析中,氨甲环酸组287位(60%)患者有良好预后,而对照组有300位(64%)(治疗中心校正的优势比 0.86,95% CI 0.66-1.12)。两组随机分组后至动脉瘤治疗前的再出血率分别为10%(氨甲环酸组)和14%(对照组)(优势比 0.71,95% CI 0.48-1.04)。两组其他重度不良反应发生情况相当。
对于CT证实的蛛网膜下腔出血患者,于超早期予以短疗程氨甲环酸治疗并不能改善其6个月内的临床预后。
原始出处:
Rene Post, et al. Ultra-early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial. The Lancet. December 21, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
32
#蛛网膜#
46
学习了
96
顶刊就是不一样,质量很高,内容精彩!学到很多
86
谢谢分享
105
1
92
太高大上了
105
学习
76