ESC 2022:冠状动脉CTA的准确性需要提高(Dan-NICAD 2)
2022-08-28 MedSci原创 MedSci原创
2022年8月28日,在ESC 2022大会 Hot Line专场上公布的最新研究,用于识别疑似冠状动脉疾病(CAD)患者的两项心肌灌注显像(MPI)的侵入性检测方式,在接受冠状动脉CT血管造影(CT
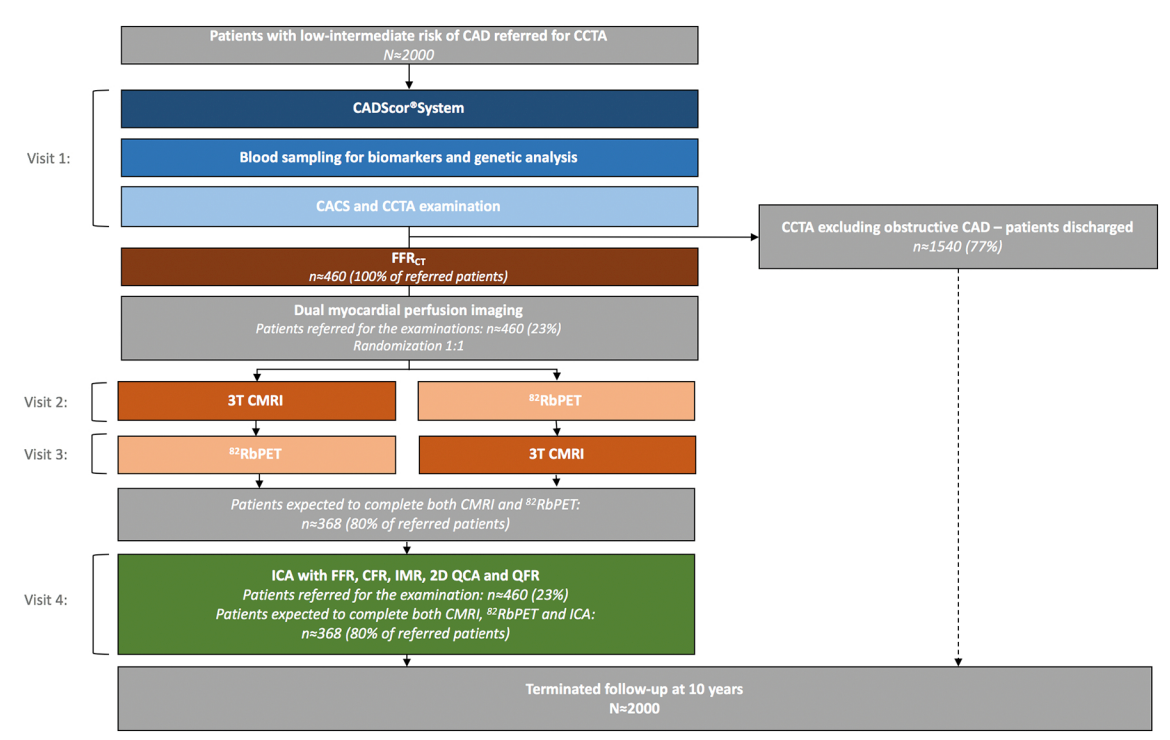
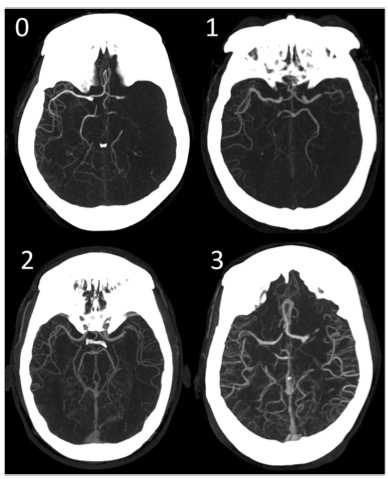
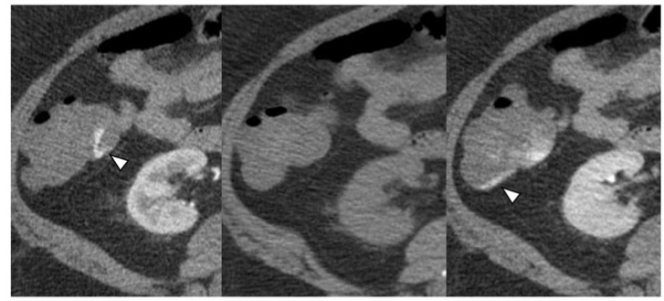
丹麦奥尔胡斯大学的Morten Bottcher教授说:“大多数转诊为冠状动脉CTA的疑似CAD患者没有阻塞性疾病。“当我们在冠状动脉CTA上发现疑似阻塞性疾病时,MPI技术被指南认可用于识别潜在血运重建的患者,然而,我们的研究结果表明,虽然这些影像学检查方法可以识别狭窄最严重和高危CAD患者,但对于普遍存在中度狭窄及血流储备分数(FFR)测试值位于灰色区域或边缘的患者而言,它们的敏感性较低。这意味着如果我们应用second-line灌注成像,许多患者可以避免有创检测。然而,这也意味着一些中度狭窄的患者被“遗漏”。因此,需要针对中度狭窄患者的诊断管理进行研究。” 经冠状动脉CTA检查,疑似阻塞性CAD的患者在转诊至侵入式冠状动脉造影(ICA)前,指南建议采用MPI验证心肌缺血。然而,关于灌注成像的表现以及这些患者中哪种灌注方式最准确的证据存在差异。Dan-NICAD 2试验使用ICA-FFR作为参考,比较了3T心脏磁共振(CMR)和82铷正电子发射断层扫描(Rb-PET)对冠状动脉CTA疑似阻塞性狭窄患者压力MPI的诊断性能。 该试验包括1732例连续出现阻塞性CAD症状并行冠状动脉CTA的患者。平均年龄59岁,57%为男性。根据冠状动脉CTA,445例患者(26%)怀疑有狭窄(定义为直径>50%的狭窄)。所有445例患者按随机顺序转诊CMR和Rb-PET,最后所有患者均接受ICA-FFR作为参考。 共有372例患者完成了CMR和Rb PET,并纳入分析。在ICA-FFR期间,164/372(44.1%)患者发现血流动力学改变的阻塞性冠状动脉疾病。 对CMR和Rb PET的敏感性分别为59%(95%CI 51-67%)和64%(95%CI 56-71%),P=0.21;特异性分别为84%(95%CI 78-89%)和89%(95%CI 84-93%),P=0.08。两种技术的阳性(PPV)和阴性(NPV)预测值相似:CMR的PPV为76%,Rb-PET为79%,CMR的NPV为73%,Rb-PET为75%。 与CMR相比,Rb-PET的总体准确度略高(分别为78%和73%;P=0.03)。与CMR相比,Rb-PET将更多高危患者(左主干或三支血管疾病)准确归类为异常:Rb-PET 30/31(96.8%),CMR 24/31(77.4%);P=0.03。 两种方法对直径>70%的严重狭窄均有很高的敏感性:CMR 83%(95%CI 72–91%),Rb-PET 89%(95%CI 79–95%)。 Bottcher教授说:“不到一半(44%)的冠状动脉CTA检测疑似冠心病的患者通过ICA-FFR确诊为阻塞性冠心病。CMR应激和PET应激对预测FFR结果具有相对中等的敏感性和高度特异性,因此灌注试验方法似乎是安全的,因为几乎所有患有严重疾病的患者(高度狭窄,左主干和三支血管疾病)均被诊断。但是,预测低FFR的适度敏感性意味着这些先进的灌注结果与侵入性FFR之间经常存在差异。” 他总结说:“冠状动脉CTA的准确性需要提高,以便更多无梗阻性CAD的患者避免进一步的检查,这可以通过更好的CT成像质量以及更先进的成像分析(如无创FFR检测和光子计数系统)来实现。同时也可以改进灌注技术,例如通过使用CMR或15O-water PET成像系统对灌注进行定量测量。” 原始出处: https://www.escardio.org/The-ESC/Press-Office/Press-releases/More-precise-algorithms-are-needed-to-select-patients-for-invasive-coronary-testing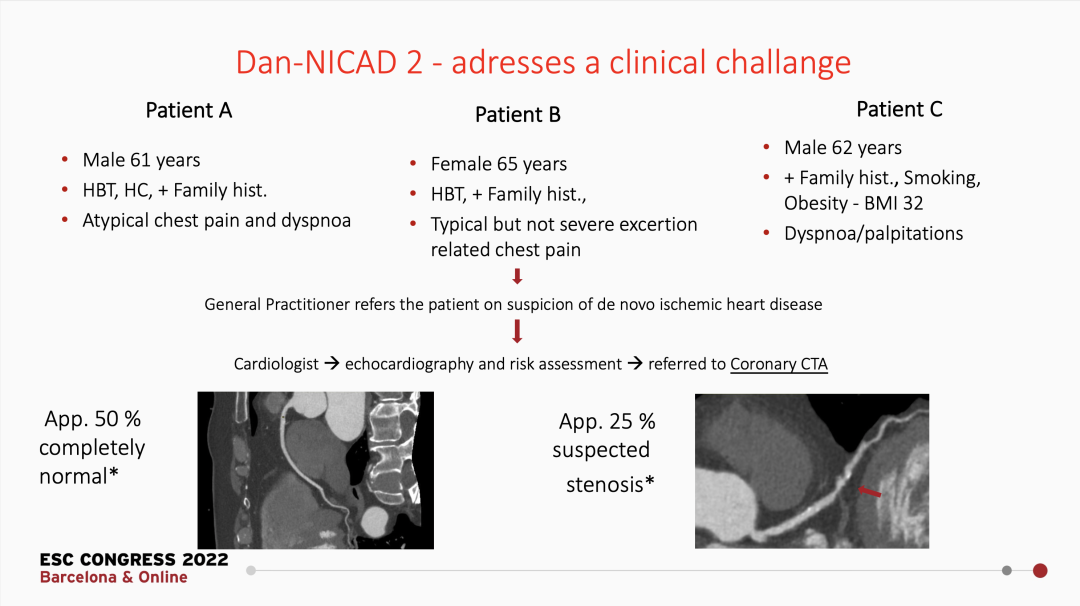

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ICAD#
50
#CTA#
50
#准确性#
47
#冠状动脉CT#
47