Heart:植入式心脏除颤器治疗的性别差异
2019-12-20 xiangting MedSci原创
在ICDs患者中,与标化设置(NID 18/24)相比,检测时间间隔长治疗室性心律失常的策略(NID 30/40)减少了男性和女性的总治疗次数。
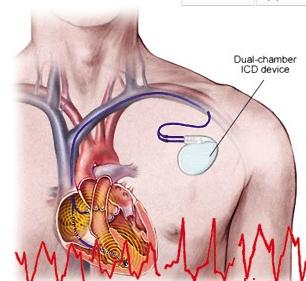
在植入式心脏除颤器(ICD)中,检测时间间隔长可以安全地减少不必要和不适当的治疗。这项研究目标是评估与男性相比,女性室性心律失常的ICD治疗,同时考虑到ICD检测。
Advance III试验将植入ICD进行一级或二级预防的患者随机分为两组,即长室性心律失常检测时间组和标化组(检测需要的间隔数量(NID)分别为30/40和18/24)。事后分析的主要终点是通过Kaplan-Meier方法和单因素Cox回归模型评估的ICD治疗发生率。
总的来说,1902例患者被随机分组(304例女性,65±11岁)。女性ICD治疗的风险较低(HR 0.63,95%CI 0.43-0.93,p= 0.022);仅在长检测时间组观察到这种差异(HR 0.37,p=0.013),而在短检测时间组没有观察到差异(HR 0.82,p=0.414)。不适当治疗和死亡率未观察到明显的性别差异。长检测时间设置明显降低了女性(总HR 0.31,p = 0.007;适当HR 0.33,p=0.033)和男性(总HR 0.69,p = 0.006;适当HR 0.73,p=0.048)的总ICD治疗和适当ICD治疗。
在ICDs患者中,与标化设置(NID 18/24)相比,检测时间间隔长治疗室性心律失常的策略(NID 30/40)减少了男性和女性的总治疗次数。女性的减少幅度更大。总体而言,与男性相比,女性接受ICD治疗的可能性更低。仅在长检测时间组中观察到该结果。
原始出处:
Maurizio
Gasparini. Sex differences in implantable cardiac defibrillator therapy
according to arrhythmia detection times. Heart. December 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#植入式#
29
#ART#
22
#除颤#
39
#植入#
27
#HEART#
24
学习了,学习了
63