Acta Anaesthesiol Scand:产妇发生意外硬脊膜穿刺后的慢性疼痛:一项病例对照前瞻性观察研究
2022-01-09 “罂粟花”公众号 “罂粟花”公众号
背景
背景
本研究调查产程中意外硬脊膜穿刺后硬脊膜穿刺后头痛(PDPH)妇女慢性头痛和背痛的发生率。
方法
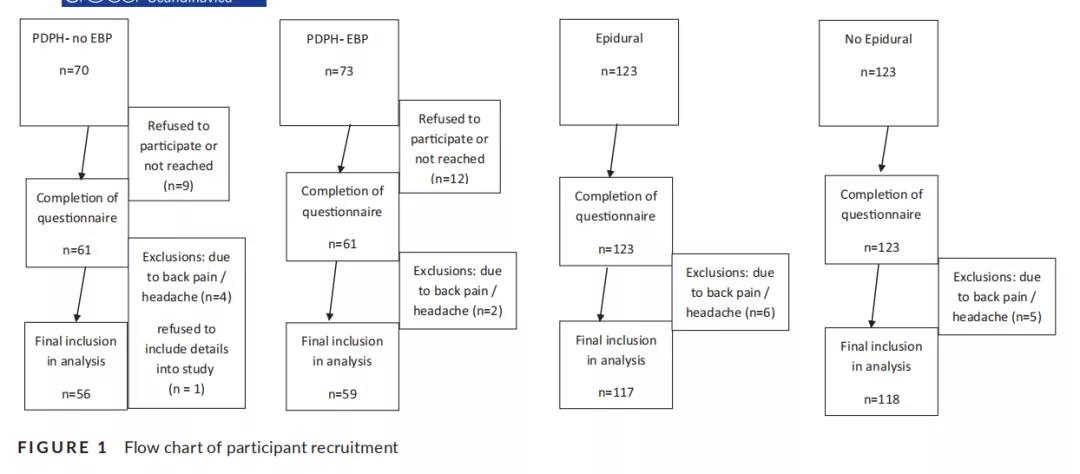
评估产后18-24个月慢性头痛、背痛和残疾的发生率。将接受硬膜外血补片(PDPH-EBP)治疗的PDPH患者与无硬膜外血补片的PDPH患者(PDPH-NO EBP)、单纯硬膜外镇痛患者和无硬膜外镇痛患者进行配对。本研究的主要结果是慢性头痛和背痛的发生率。次要结果是硬膜外补血对慢性疼痛发展的影响。本研究使用卡方检验或 Fisher's检验来计算优势比。
结果
两组之间的人口统计特征没有统计学意义。在非硬膜外组中,没有女性发生慢性头痛,2/116例(1.7%)发生慢性背痛。在无并发症的硬膜外组中,无女性发生慢性头痛,7/116(6.0%例)报告慢性背痛。在PDPH-NO EBP组中,9/56(16.1%)妇女报告慢性头痛,10/56(17.9%)报告慢性背痛。PDPH-EBP组慢性头痛12/59例(20.3%),慢性腰背痛14/59例(23.7%)。无硬膜外或无并发症硬膜外组无残疾报告(慢性疼痛评分为3或4)。PDPH-no EBP组和PDPH-EBP组分别有8.9%和8.4%的女性报告高度残疾。

结论
患有PDPH的女性有较高的慢性头痛、背痛和残疾的发生率。本研究发现保守治疗和EBP治疗的患者在慢性疼痛发展方面的差异没有统计学意义。
原始出处:
Binyamin Y, Heesen P, Orbach- Zinger S, et al. Chronic pain in parturients with an accidental dural puncture: A case- controlled prospective observational study. Acta Anaesthesiol Scand. 2021;00:1– 8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#对照#
29
#病例对照#
54
#观察研究#
32
#CTA#
32
#EST#
31
#前瞻性#
20
#硬脊膜穿刺#
33
#ANA#
21
#慢性疼痛#
0
#穿刺#
46