Circulation:抑制脑啡肽酶对MI后左室收缩功能障碍患者的心室重构的影响
2021-05-17 Nebula MedSci原创
在心肌梗死后出现无症状左心室功能减退的患者中,与缬沙坦相比,Sacubitril/缬沙坦治疗没有显著的抗心室重构效果
心肌梗死(MI)后出现左心室收缩功能不全(LVSD)的患者随后发生心力衰竭(HF)的风险较高。左心室重构,即左心室渐进性扩张、每搏量逐渐减少,可促使患者在MI后几年、数周甚至数天内发生HF。

鉴于脑啡肽酶的底物具有舒张血管、抗肥厚、抗纤维化和交感神经溶解作用,在抑制肾素血管紧张素系统(RAS)的同抑制脑啡肽酶(neprilysin)或可减轻不良左室重构。
这是一项前瞻性、多中心、随机、双盲、主动比较试验,招募了心肌梗死后超过3个月的LV射血分数(LVEF)≤40%且在服用RAS抑制剂(雷米普利≥2.5 mg·2次/日的等效剂量)的患者,对比了采用Sacubitril/缬沙坦97/103 mg和160 mg缬沙坦的比较治疗的预后。主要结果是使用心脏磁共振成像(MRI)测量的左室收缩末期容积指数(LVESVI)从基线到第52周时的变化。次级结果包括左室重构的其他MRI测量、NT-proBNP和高敏感性心肌肌钙蛋白I (hs-TnI)的变化,以及患者整体变化评估问卷。
从2018年7月到2019年6月期,共有93名患者被随机分至两组:平均60.7±10.4岁,中位MI时间为3.6年(IQR 1.2-7.2),平均LVEF为36.8%±7.1,中位NT-proBNP水平为 230pg/mL(124-404)。
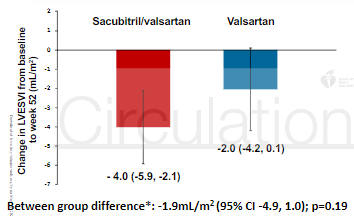
两组LVESVI的变化
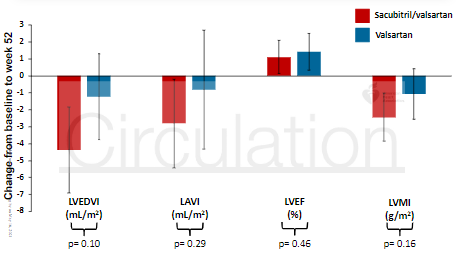
与缬沙坦相比,Sacubitril/缬沙坦并没有显著降低患者的LVESVI:校正组间差异-1.9mL/m (95%CI -4.9~1.0);p=0.19。NT-proBNP、hs-TnI、左室舒张末期容积指数、左房容积指数、LVEF、左室质量指数、患者整体变化评估组间差异均无统计学意义。
第52周时,两组各指标的变化
综上所述,在心肌梗死后出现无症状左心室功能减退的患者中,与缬沙坦相比,Sacubitril/缬沙坦治疗没有显著的抗心室重构效果。
原始出处:
Docherty Kieran F,Campbell Ross T,Brooksbank Katriona J M et al. The Effect of Neprilysin Inhibition on Left Ventricular Remodeling in Patients with Asymptomatic Left Ventricular Systolic Dysfunction Late After Myocardial Infarction.[J] .Circulation, 2021, https://doi.org/10.1161/CIRCULATIONAHA.121.054892
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脑啡肽酶#
40
#收缩功能障碍#
31
#左室收缩功能障碍#
43
#心室重构#
38
#功能障碍#
29