主题:心肌淀粉样变
左心室肥厚的鉴别诊断?
心肌淀粉样变的临床分型?
心肌淀粉样变的诊断及治疗思路?
患者 刘某,58岁,
籍贯:四川 洪雅县
无心血管疾病相关家族史
主诉:活动后胸闷气紧1年,心脏骤停1次
现病史:患者于2016-01-18入住我院。入院前1年患者活动后出现胸闷气紧,持续约几分钟,经休息后可缓解,患者未重视,未进一步诊断治疗。入院前8天,患者夜半如厕时出现头晕,站立不稳,随后意识丧失,持续约1 min后症状自行缓解。患者遂至当地县医院就诊,诊断为“1.冠心病全心衰竭心功能Ⅲ级;2.肾病综合征 3.肺部感染”,予抗感染,控制心率,利尿等治疗,患者住院期间再次出现心悸、晕厥,心电图示“心室颤动、心脏骤停”,经紧急气管插管、心肺复苏成功后急诊转至我院治疗。
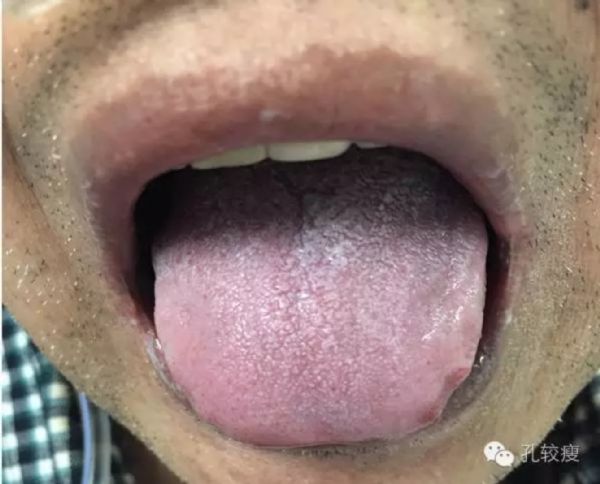
入院查体:体温36.3℃,脉搏65次/min,呼吸20次/min,血压106/68 mm Hg(1 mm Hg=0.133 kPa),发育正常,营养中等,神志清晰,精神差。全身皮肤黏膜无黄染、瘀点、瘀斑,湿度、弹性正常。全身浅表淋巴结未扪及肿大。双侧眼睑无水肿,结膜无水肿、充血,巩膜无黄染;口唇轻度紫绀,口周无疱疹,舌体稍胖大,舌边较多齿痕(下图)。颈部形态正常,活动自如,颈静脉无充血、怒张,肝颈静脉反流征(-);双下肺闻及少许干鸣音,双上肺闻及少许湿啰音。心尖搏动正常,心界向两侧扩大,心率为65次/min,律齐,各瓣膜听诊区未闻及杂音。腹软,无压痛、反跳痛,肝脾肋下未扪及,双肾区无叩击痛,移动性浊音(-),肠鸣音正常,双下肢轻度水肿。生理反射存在,病理反射未引出。
图 患者舌体稍大,边缘可见齿痕
入院心电图检查见下图,后多次复查心电图,其ST段均未见动态变化;动态心电图示:偶发房早,多源性室性早搏,偶有二联律,偶有成对出现,偶有短阵室性心动过速。
图1 入院心电图提示肢体导联明显电压(没骗你吧,QRS波比P波还小)
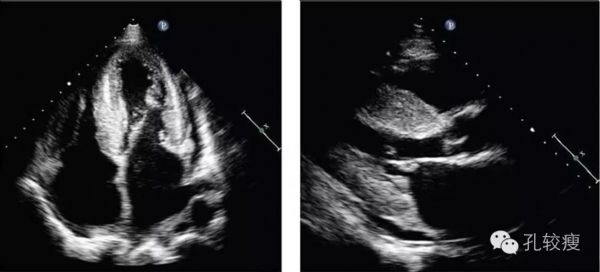
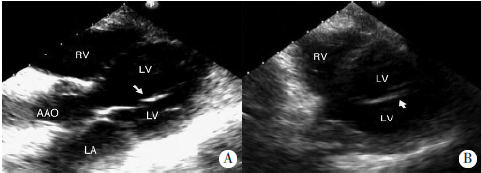
心脏彩色多普勒超声示左心房(40 mm)及右心房(47mm×52mm)增大,室间隔(23mm)、左心室后壁(23mm)明显增厚,心肌内见颗粒状强回声。二、三尖瓣轻度反流,二尖瓣前瓣环组织多普勒e’峰>a’峰;左心室射血分数46%,心包少量积液(下图)。
图2 心尖四腔心切面及左心室长轴切面示双心房增大,左心室肥厚。
图3 左心室短轴切面示左心室明显肥厚,心肌内见颗粒状强回声,组织多普勒示左心室呈限制性充盈障碍
心肌肥厚的鉴别诊断
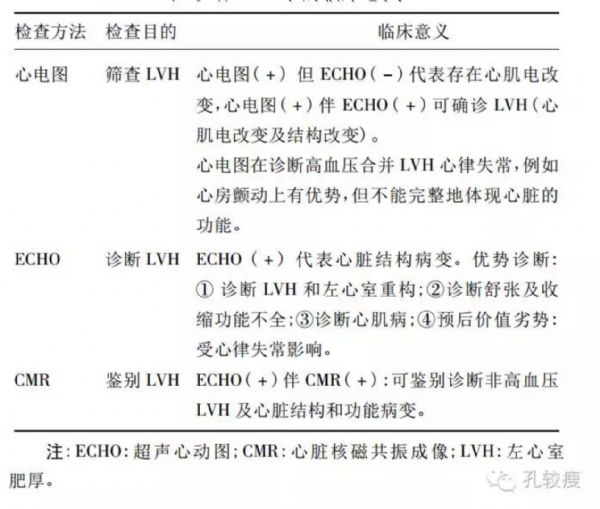
左心室肥厚是临床常见征象,无论是超声医师、心电图医师还是磁共振医师,均对该异常具备诊断标准。但我们不可否认,有时心电图、磁共振和心脏超声的表现往往并不完全统一。下方表格中,我们列举了三种常见诊断和手段在诊断左心室肥厚中的意义。大家可以看到心电图在左心室肥厚中所起的作用是筛查、超声心动图提供的是诊断、磁共振是病因鉴别,三者各司其职,各有优劣。
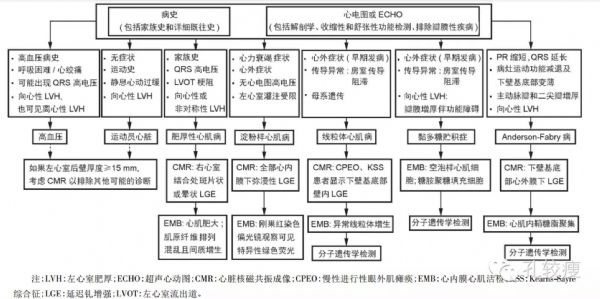
患者中年男性,以活动耐量下降、心脏骤停为主要临床表现,超声心动图提示双心房增大伴左心室肥厚;以此为切入点进行诊断及鉴别诊断。心肌肥厚在临床上一般可分为获得性和遗传性两大类。获得性心肌肥厚包括血流动力学障碍(如高血压,主动脉瓣狭窄,主动脉缩窄)及内分泌疾病(生长激素过多、嗜铬细胞瘤等)。本例患者无高血压、瓣膜病病史,且无巨人症及嗜铬细胞瘤表现,故可基本排除上述获得性因素所致。遗传性心肌病包括肥厚型心肌病及代谢性或者贮积型疾病。前者系编码心肌节蛋白的基因突变导致以左心室肥厚为特征的原发性心肌病,常常伴有左心室高电压等心电图改变。该例患者虽存在有心室肥厚,但心电图却表现为肢体导联低电压,故考虑为浸润性心肌病变,如心肌淀粉样性、Fabry病等;总结该患者病史特点:
患者为中年男性,临床表现以心脏、肾脏两个器官功能病变为主。
体格检查提示存在舌体胖大、舌边有齿痕。
心脏超声提示心肌肥厚,肌肉内部可见颗粒性回声。
肢体导联重度低电压趋势。
综上,患者存在浸润性心肌病尤其是心肌淀粉样变的可能性很大。
左心室肥厚的鉴别诊断思路
心肌淀粉样变分型及鉴别诊断
轻链型心肌淀粉样:为最常见的心肌淀粉样变,是由于单克隆轻链(λ或κ)浓度增高所致。需要排除患者血和尿无单克隆轻链增高,多伴有多发性骨髓瘤,为明确诊断需要检查骨髓浆细胞形态和比例。
继发型心肌淀粉样变:系由淀粉样A蛋白在心肌沉积所致的一类疾病,非常少见,主要继发于慢性感染、肿瘤或自身免疫性疾病。该患者没有上述疾病,因此可除外继发型心肌淀粉样变。
老年性心肌淀粉样变:是由于甲状腺素转运蛋白(TTR)在心肌异常沉积所致,主要见于80岁以上患者,60岁以下罕见。本患者年仅35岁,因此不考虑老年性心肌淀粉样变的诊断。
血透相关性心肌淀粉样变:见于长期血透患者。由于透析不能清除血液中的β2微球蛋白,异常升高的β2微球蛋白沉积在心脏导致该病形成。该患者无血透史,因此可除外该病。
遗传性心肌淀粉样变:相对常见于青年人,是由于编码TTR基因突变,导致功能异常的TTR在心脏沉积所致。根据该患者的病史,尚不能排除遗传性心肌淀粉样变,需要和轻链型鉴别。
安排相关检查
血常规示白细胞13.13×109/L,中性粒细胞数10.53×109/L,中性粒细胞百分比80.2%,C反应蛋白23.9(0~8)mg/L
乳酸脱氢酶431(109~245)U/L,
血全套示D-二聚体:1.39(0~1) mg/L,血浆纤维蛋白原7.53(2.0~4.0)g/L,血清电解质未见异常,肌酐176(55~87)umol/L,尿素氮14.65(3.1~8.0)mmol/L,白蛋白26(40~55)g/L;
尿蛋白(+++),尿蛋白定量4.51 g/24 h
输血前全套及甲状腺功能未见异常。
血清蛋白电泳示白蛋白44.9(60~71)%,α1球蛋白3.6(1.4~2.9)%,α2球蛋白20.9(7.0~11.0)%,β球蛋白11.1(8.0~13.0)%,γ球蛋白2.7(9.0~16.0),M蛋白16.8%,提示存在M蛋白血症。
免疫球蛋白定量示IgG11.20%(7~16)%,IgA 0.53%(0.7~4.0)%,IgM 0.45%(0.5~2.20)%,KAP轻链0.52%(1.7~3.7)%,LAM轻链3.39%(0.9-2.1)%,KAP/LAM=0.15。
尿本周蛋白测定为阳性,尿KAP轻链0.04 g/L,LAM 0.26g/L。后行血清免疫固定蛋白电泳以及尿本周蛋白电泳示IgG-LAM轻链型M蛋白血症(下图)。
血清免疫固定电泳结果:电泳图上有一条M蛋白带(黑箭头),与抗IgG和抗L形成特异性反应沉淀带(白箭头)
尿本周蛋白免疫固定电泳结果:电泳图上有一条M蛋白带(黑箭头),与抗GAM、抗L形成特异性反应沉淀带(白箭头)
行腹部脂肪活检,示病变组织光镜下呈无定型、均匀的嗜伊红物质,用刚果红染色在偏光显微镜下呈典型绿色双折光,患者诊断为轻链型心肌淀粉样变。结合患者肾功能改变,考虑淀粉样变同样累及肾脏。
M蛋白血症鉴别诊断
根据病因,M蛋白血症可分为多克隆性(反应性)及单克隆性(肿瘤性)两种。该患者无慢性肝病、慢性迁延性感染、结缔组织病等,结合其尿本周蛋白阳性,考虑为多发性骨髓瘤(浆细胞病)可能性大。
患者行头颅及骨盆X线平扫未见确切骨质破坏;为进一步明确诊断,遂行骨髓涂片及活检示:造血组织增生不均一,增生区粒红巨三系降低,浆细胞增生,比例约55%,细胞免疫表型示CD38(+),CD56(+);确诊为多发性骨髓瘤(下图)。
患者入院后经过利尿、纠正心衰,抗感染等对症治疗,症状逐渐好转。邀请血液科会诊后,建议给予美法仑、泼尼松、沙利度胺(MPT方案)化疗。
骨髓涂片浆细胞明显增生,见胞浆深染呈灰蓝色,部分呈多核,偶见Russel小体;骨髓活检示增生区粒红巨三系降低,浆细胞单克隆性增生
孔较瘦有话说
合并有多发性骨髓瘤的心肌淀粉样,其临床预后极差。早期发现并启动原发病治疗有助于改善预后。临床中,当患者合并以下特点时,应该高度怀疑淀粉样变心肌病:①心室腔不大伴进行性难治性心力衰竭; ②左心室肥厚伴心电图低电压; ③既往有高血压伴进行性低血压及类似陈旧性心肌梗死图形;④左心室壁均匀肥厚伴室壁活动弥漫性减低;⑤舌体宽大肥厚伴齿痕。
鉴于本患者多次发生恶性心律失常,建议积极药物治疗,如病情好转则计划择期行植入性心脏除颤复律仪治疗(指南中推荐级别不高)。
手术前一日,患者再次突发意识丧失,小便失禁,心电监护示心室颤动,经积极抢救无效后死亡。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#心室肥厚#
35
#肢体导联#
27
好文章学习了
71
#左心室肥厚#
44
#左心室#
0
#鉴别诊断#
24
学习了
72
学习一下
75
好文献学习了
64