Cell :液体活检再获突破!全新生物标志物可早期诊断多种癌症
2020-08-19 药明康德内容团队 学术经纬
很多研究癌症的科学家希望能够在癌症患者的早期阶段就做出准确的诊断,帮助患者赢得治疗时间。顶尖学术期刊《细胞》近日在线发表了一项有关液体活检的新研究,为癌症早期诊断带来了潜在的全新方法。
顶尖学术期刊《细胞》近日在线发表了一项有关液体活检的新研究,为癌症早期诊断带来了潜在的全新方法。
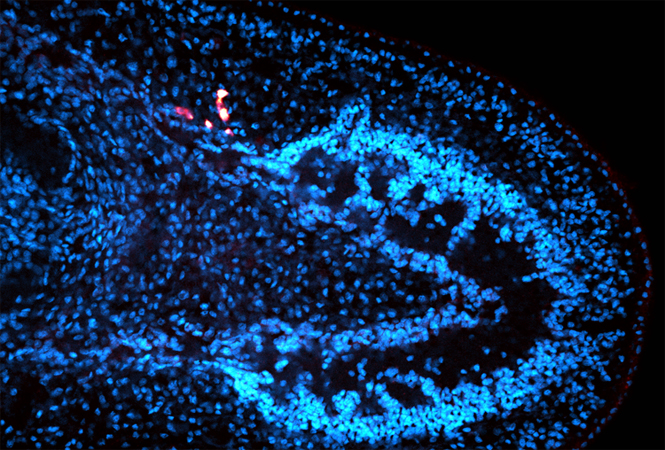
来自纪念斯隆-凯特琳癌症中心(MSK)和威尔·康奈尔医学研究所(Weill Cornell Medicine)的研究团队报告说,由肿瘤和免疫细胞释放的细胞外囊泡和颗粒(extracellular vesicles and particles,简称EVP),携带可靠的生物标志物,可用于癌症检测,并确定癌症的类型。
“一小管血液中就含有数十亿EVP,这意味着,癌症患者有大量的癌症相关EVP可供临床医生用来诊断。”这项研究的共同通讯作者David Lyden教授介绍。
癌症是全世界范围内最主要的死亡原因之一,每年都夺走了无数人的生命。很多研究癌症的科学家希望能够在癌症患者的早期阶段就做出准确的诊断,帮助患者赢得治疗时间。同时,这样的检查方法还要简单方便,避免让患者感到痛苦。
“液体活检”技术应运而生。顾名思义,这类技术想要通过检查各种体液,来检测癌症和监测疾病进展。其中,最常见的液体活检形式是检测和分析癌细胞释放到血液中的DNA。利用这类技术进行癌症早筛目前还在开发和临床验证阶段。
这项新研究则另辟蹊径,不是分析DNA片段,而是侧重于检查EVP中包含的各种蛋白质。
EVP是细胞分泌的小颗粒,大小只有纳米级别。它们像快递包裹一样,外层有膜,里面可以装RNA、DNA、蛋白质、代谢产物和脂质等活性分子。这些小包裹可以介导细胞间信号传导,调节基质组织,甚至调节炎症和免疫反应,还可以穿越诸如血脑屏障之类的屏障,并以高度的特异性被“吞”入细胞。
Lyden教授的研究团队发现,肿瘤在生长、转移的过程中同样会释放EVP,并以这种方式通知身体的其他部位做好迎接癌细胞的准备。因此,理论上通过检查不同EVP的内容物,可以推断出癌症的信息。
在这项研究中,科学家们验证了初步的想法。他们收集了400多份人类组织、血液和其他体液样本,涵盖了18种不同的癌症,如乳腺癌、结肠癌、肺癌、胰腺癌等,并且包括了早期在内的不同癌症阶段,以及作为对照的健康样本。然后,通过基于质谱的蛋白质组学方法,分析了EVP中的蛋白质。
研究人员首先比较了组织样本中肿瘤和邻近组织的EVP蛋白质组,确定哪些EVP蛋白可以用作癌症诊断标志物。利用这些特征性的蛋白区分肿瘤和正常组织,可以达到95%的敏感性和94%的特异性。
当然,要做液体活检,血液是最方便进行检测的样本之一。因此,研究人员接下来通过匹配来自组织样本和血浆中的EVP,进一步找出了癌症患者血浆中独特的肿瘤相关EVP蛋白。应用机器学习分类,研究人员将血浆EVP中的特定蛋白(例如免疫球蛋白)与癌症类型相匹配。经验证,这种方法检测癌症的敏感性可达到95%,特异性达到90%。
值得一提的是,对于一些诊断结果为“原发位置不详的肿瘤”,根据血浆中EVP携带的特征性蛋白,也可以对这些肿瘤做出分类。
研究人员指出,尽管在确认肿瘤位置时仍然需要进行CT和MRI扫描,但可以利用血液检查来确定是否患癌已经是一个巨大的进步。展望未来,研究团队希望可以在更多临床样本上验证这套新方法。
共同通讯作者William Jarnagin博士指出,有一些癌症目前还没有筛查方法可以及早发现,例如肝癌和胰腺癌,这类新型的检测方法或许可以提供帮助,让患者尽早治疗改善预后。他说:“这项研究是一项概念验证,在把它作为筛查工具之前,我们还有许多工作要做。但如果我们最终能应用这种方法在患者出现症状之前就发现癌症,那就太棒了。”
希望在不久的将来,检测癌症就可以像验血一样容易,做到早发现,早治疗,把癌症扼杀在萌芽之中。到了那个时候,我们再也不会因为没有及时发现亲人的癌症,而抱憾终身。
原始出处:
Ayuko Hoshino, Han Sang Kim, Linda Bojmar, et al.Extracellular Vesicle and Particle Biomarkers Define Multiple Human Cancers.Cell. 2020 Aug 11;S0092-8674(20)30874-6. doi: 10.1016/j.cell.2020.07.009.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
34
#CEL#
40
#标志物#
27
#活检#
36
#早期诊断#
43
#生物标志#
28
#生物标志#
45
很好
0
看原文
99
#液体活检#极有前途的检测方法
0