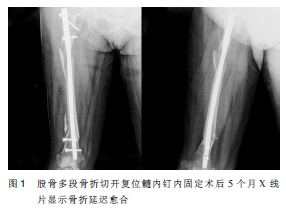
微创钢板内固定治疗股骨干多段骨折髓内钉内固定术后骨折延迟愈合1例
2019-01-28 康立恒 中国骨与关节损伤杂志
强大暴力导致的复杂多段粉碎性骨折占股骨干骨折的3%~7%。交锁髓内钉内固定是治疗股骨干骨折的金标准,但在临床上仍有部分患者术后出现骨折不愈合。Shroeder等报道交锁髓内钉内固定术后骨折不愈合的发生率为1.1%~12.5%。股骨干多段骨折波及范围广,靠近股骨粗隆下的骨折,骨折近端受到髂腰肌牵拉的作用,向前方移位明显,闭合复位难度较大,往往需要小切口辅助复位,因而破坏髓外血供,增加骨折延迟愈合及不

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#股骨干多段#
35
#股骨干#
36
微创钢板内固定治疗。
67
微创钢板内固定治疗。
71
#微创#
27
#髓内钉#
31
#股骨#
30
#内固定#
29
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
79