European Radiology:定量MRCP(MRCP+)对原发性硬化性胆管炎风险分层的评价
2022-01-20 shaosai MedSci原创
原发性硬化性胆管炎(PSC)是一种进展性的肝脏和胆道自身免疫性疾病,在男性中更为流行,一般与炎症性肠病(IBD)有关。
原发性硬化性胆管炎(PSC)是一种进展性的肝脏和胆道自身免疫性疾病,在男性中更为流行,一般与炎症性肠病(IBD)有关。该疾病的病理特征是造成胆管的局灶性狭窄和扩张,最终导致继发性肝硬化和肝胆肿瘤的发生。到目前为止,PSC还没有有效的治疗方法,在大多数情况下会发展成肝衰竭,甚至导致死亡或肝移植。
PSC的诊断主要通过磁共振胆囊造影(MRCP)来确定,通常不需要结合患者的临床和生化情况进行肝脏活检,因此存在较大的局限性。MRCP是目前一线的无创诊断工具,基本上只能对胆道树进行定性评估,而这种评估往往受制于观察者之间的差异。现阶段,临床上建立了ANALI 1和2分数,为MRCP图像提供一个标准化的判析结构。尽管这些分数已被证明与影像学疾病进展和临床预后有关,但其仍不能克服MRCP的定性性质。最近,有学者建议使用一种半自动软件,对三维MRCP图像进行定量分析(MRCP+),以提供更准确的诊断和评估。
近日,发表在European Radiology杂志的一项研究通过评估各种MRCP+参数与已建立的生化风险评分(MRS、AOPI和PREsTo)的关联,评估了其对患者临床风险分层的能力;同时还评估了MRCP+与MRE的性能,以评估MRCP+与现有形态学MRCP评分(如ANALI 1和ANALI 2)结合使用时的附加价值,为临床提供了一种能够精确量化胆管潜狭窄和扩张的影像学技术,有助于实现疾病的有效管理和肿瘤监测。
本研究于2014年1月至2015年12月期间回顾性评估了65名PSC患者的MRI图像、通过MRE测量肝脏硬度以及生化检测。MRCP+被用来对MRCP图像进行后处理,以获得胆管和胆道树的定量测量。线性回归分析被用来检验关联。采用Bootstrapping作为验证方法。
节段性狭窄的总数与Mayo风险评分的关联最强(R2 = 0.14),最小狭窄直径与Amsterdam Oxford预后指数的关联最高(R2 = 0.12),宽度为0-3毫米的胆管结节百分比与PSC风险估计工具的关联最强(R2 = 0.09)。存在中位数>9毫米的胆管与MRE的关联度最高(R2=0.21)。MRCP+与Mayo风险评分的关联强度与ANALI2相当,弱于MRE(分别为R2=0.23,0.24,0.38)。MRCP+增强了ANALI 2和MRE与Mayo风险评分的关联。
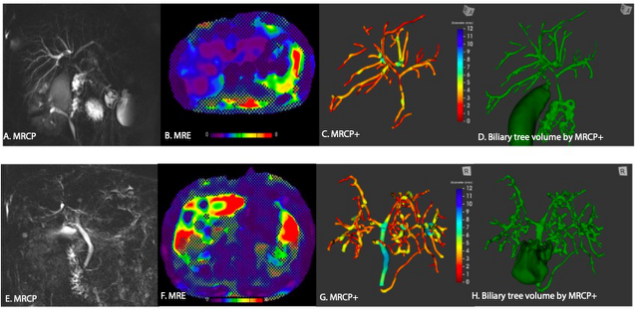
图 低(A-D)和高(E-H)Mayo风险分数的PSC患者,展示了MRCP(A,E)、MRE(B,F)、MRCP+(C,G)和MRCP+(E,H)得出的胆管差异。Mayo风险评分高的患者在MRCP和MRCP+上显示出更大的弥漫性肝内胆管狭窄,在MRE上肝脏硬度增加,在MRCP+上胆管树体积增加。
本研究表明,MRCP+参数可通过与生化风险评分、ANALI和MRE的联系对PSC患者进行风险分层。此外,MRCP+与ANALI和MRE的结合改善了与MRS的关联。最后,MRE和MRCP+的结合可以对诊断时和随后的随访中用于评估PSC的胆管和肝脏部分的影像学证据进行客观量化。
原文出处:
Marwa F Ismail,Gideon M Hirschfield,Bettina Hansen,et al.Evaluation of quantitative MRCP (MRCP+) for risk stratification of primary sclerosing cholangitis: comparison with morphological MRCP, MR elastography, and biochemical risk scores.DOI:10.1007/s00330-021-08142-y
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#原发性#
46
#PE#
38
#风险分层#
39
#原发性硬化性胆管炎#
67
#评价#
38
#硬化性#
32
#胆管#
30