Eur Urol Focus:钬激光和铥激光前列腺切除术:随机对照试验的系统回顾和元分析
2021-04-29 AlexYang MedSci原创
钬激光(HoLEP)和铥激光(ThuLEP)是最常用于内窥镜下前列腺切除术的两种方法。目前仍不清楚这两种方法在疗效和并发症方面哪个表现更好。
钬激光(HoLEP)和铥激光(ThuLEP)是最常用于内窥镜下前列腺切除术的两种方法。目前仍不清楚这两种方法在疗效和并发症方面哪个表现更好。

最近,有研究人员比较了HoLEP和ThuLEP的围手术期和功能结果。
研究人员根据Cochrane合作组织的建议并按照PRISMA标准进行了系统回顾和元分析。根据PICO标准,研究人员进行了全面的数据库检索,包括MEDLINE、Web of Science、CINAHL、ClinicalTrials.gov和CENTRAL。研究只考虑随机对照试验(RCTs)。检索发现了556项研究,其中4项符合定性和定量分析的条件,其中共报告了579名患者,随访时间长达18个月。在ThuLEP和HoLEP之间,研究人员没有观察到手术时间、切除重量、导管插入时间或住院时间的明显差异。ThuLEP的血红蛋白下降明显较低(平均差异为-0.54 g/dl,95%CI:-0.93至-0.15;P<0.001),但证据的确定性较低。暂时性尿失禁在HoLEP中更为常见(OR 0.56,95%CI为0.32-0.99;P=0.045),但同样证据的确定性较低。此外,在其他并发症或功能测量和症状评分方面没有观察到显著差异。
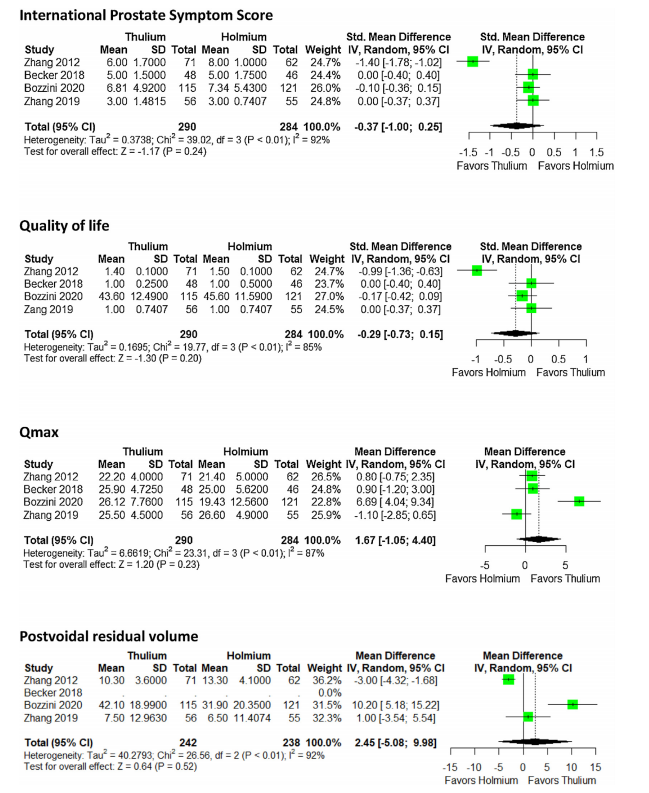
最后,研究人员指出,ThuLEP和HoLEP对症状和术后排尿参数的改善是相当的。两种手术都很安全,主要的并发症也很罕见。ThuLEP在失血量和暂时性尿失禁的发生率方面显示出轻微的优势。由于证据的确定性较低,对此应谨慎解释。因此,治疗选择应基于外科医生的专业知识和当地条件进行。
原始出处:
Friedrich O Hartung , Karl-Friedrich Kowalewski , Jost von Hardenberg et al. Holmium Versus Thulium Laser Enucleation of the Prostate: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照试验#
36
#前列腺切除#
45
#元分析#
46
#对照#
34
#切除术#
46
#激光#
37
#随机对照试验#
36
#系统回顾#
39
高质量研究,读起来真爽,谢谢梅斯
57