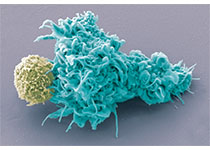
Cell:刷新认知!癌细胞竟会放出“无人攻击机”,远程破坏免疫系统总部
2019-04-05 佚名 学术经纬
今天,顶尖学术期刊《细胞》上发表了一篇重量级的论文。来自加州大学旧金山分校(UCSF)的科学家们发现,我们现有关于癌症免疫疗法的认知,很有可能是不完善的……其实不用这些科学家提醒,我们就知道现在的免疫疗法存在短板。“在黑色素瘤等最佳治疗案例中,免疫检查点抑制剂也只能对20%-30%的患者生效。在类似于前列腺癌等其他癌症里,缓解率只有个位数,”本研究的负责人Robert Blelloch教授说道:“

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
29
#Cell#
25
厉害了我的哥
71
#癌细胞#
27
s
79
免疫疗法,外泌体
76