Cancer Cell:复旦大学绘制全球很大三阴性乳腺癌多组学精细图谱!
2019-03-24 Paris 转化医学网
作为红颜杀手,乳腺癌实则已进入分类治疗时代,芳香化酶抑制剂耐药的激素受体阳性乳腺癌患者,CDK4/6抑制剂、氟维司群等药物提供新的可能,人表皮生长因子受体-2(HER-2)阳性乳腺癌患者的抗HER-2靶向新药不断问世显着改善其预后及生存。
导 读
作为红颜杀手,乳腺癌实则已进入分类治疗时代,芳香化酶抑制剂耐药的激素受体阳性乳腺癌患者,CDK4/6抑制剂、氟维司群等药物提供新的可能,人表皮生长因子受体-2(HER-2)阳性乳腺癌患者的抗HER-2靶向新药不断问世显着改善其预后及生存。而三阴性乳腺癌(TNBC)因无治疗性靶点,持续困扰着广大女性患者。相较其他亚型,其对新辅助化疗反应良好,不过残留病灶复发率极高,而且TNBC有6种亚型,不同类型具有不同的治疗反应和预后。因此,TNBC的精确分类对于实现个性化治疗十分重要。今由复旦大学附属肿瘤医院等四支专家团队历时五年联合攻关,绘制出全球最大的三阴性乳腺癌队列多组学图谱,并提出“三阴性乳腺癌分子分型基础上的精准治疗策略”。该研究今日在线发表在影响因子高达22的医学期刊《Cancer Cell》杂志上。
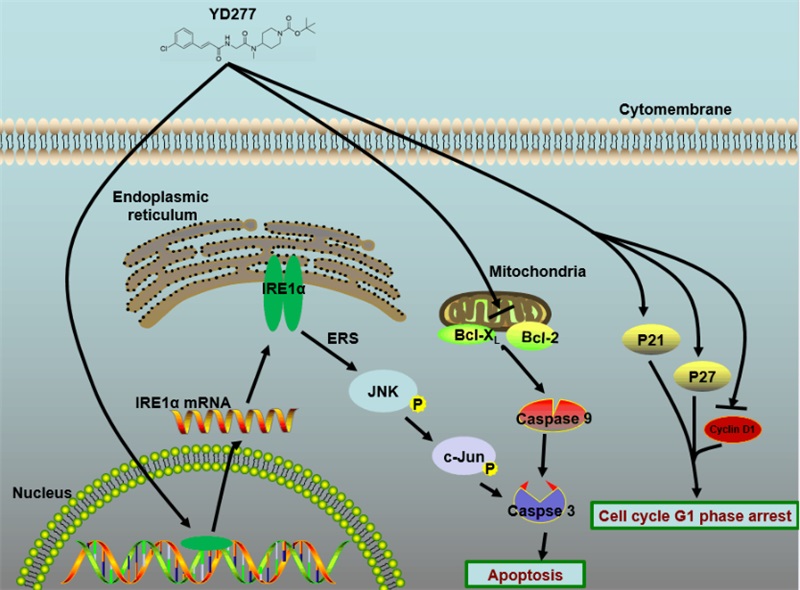
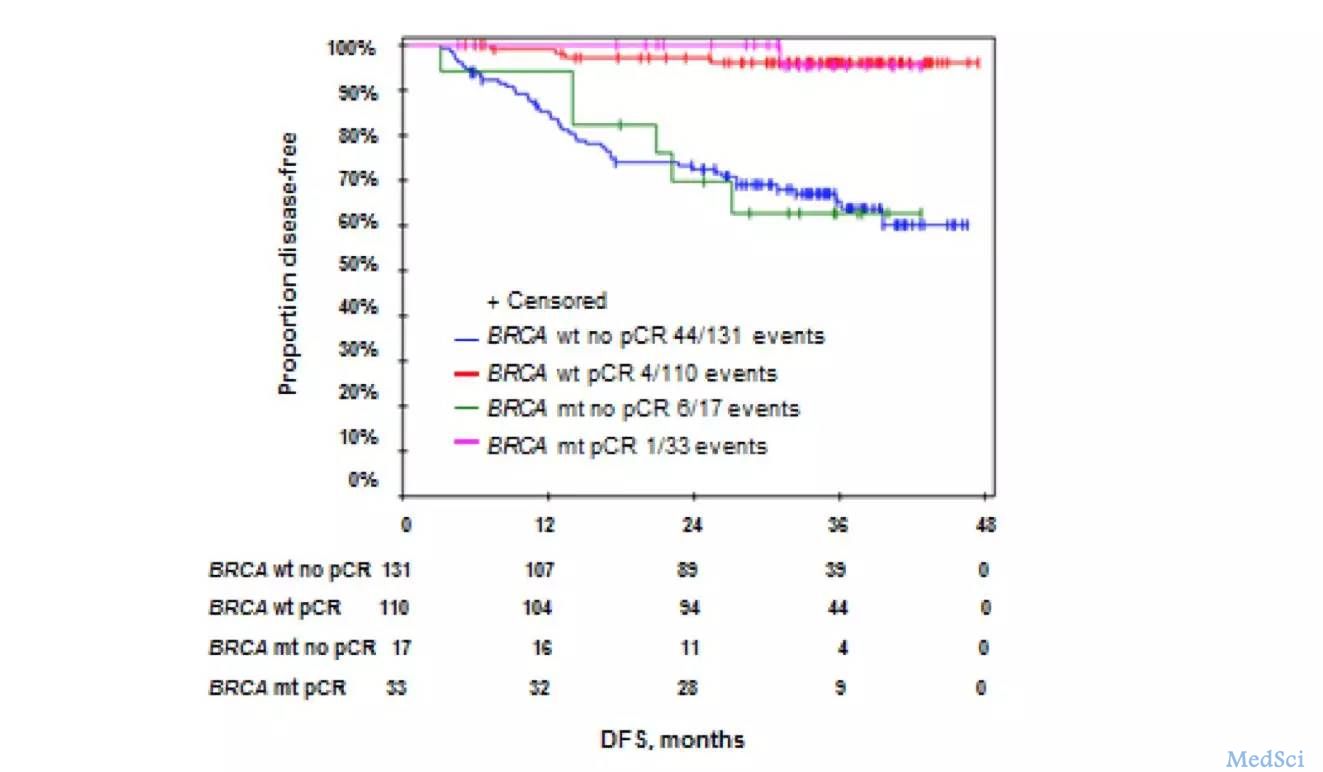
三阴性乳腺癌之所以称为‘三阴’,正是因为这种乳腺癌的亚型雌激素受体、孕激素受体和HER-2三个主要治疗靶点均为阴性。在此前的研究中,研究人员发现,基底样型TNBC高表达细胞周期和DNA损失相关基因,对顺铂敏感;间叶细胞型和间充质干细胞型的TNBC上皮间质转化(EMT)活跃,表现出对PI3K/mTOR通路抑制剂和达沙替尼(dasatinib)敏感;雄激素受体型的TNBC存在雄激素受体(AR)信号通路和PI3K通路的活化,表现出对AR抑制剂和PIK3CA抑制剂敏感;免疫调节型大多存在肿瘤相关淋巴细胞浸润(TIL)和免疫相关分子的表达,可能对免疫治疗,如PD-1/PD-L1抑制剂、肿瘤疫苗等表现出更为敏感的特性。进一步探索发现,预后差的三阴性乳腺癌,可以采用靶向治疗联合化疗的策略,以改善治疗效果。
基于以上研究思路,借助测序技术,研究团队通力合作,对465例三阴性乳腺癌标本展开研究,通过大量数据的比对分析,根据这些亚型表面蛋白的不同特征,他们将三阴性乳腺癌分类,并命名为4个不同的亚型:免疫调节型、腔面雄激素受体型、基底样免疫抑制型、间质型。并绘制出三阴性乳腺癌的基因图谱。这是国际上首次基于多维组学大数据系统提出的三阴性乳腺癌分类标准。
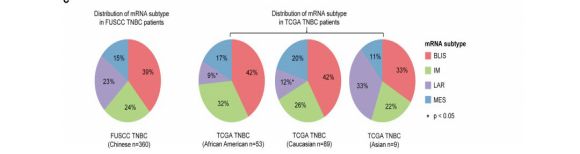
同时,此项研究还首次公布了一批中国人三阴性乳腺癌的特有基因突变:例如PIK3CA基因突变,在我国三阴性乳腺癌患者人群中的比例要显着高于美国的数据。研究表明:
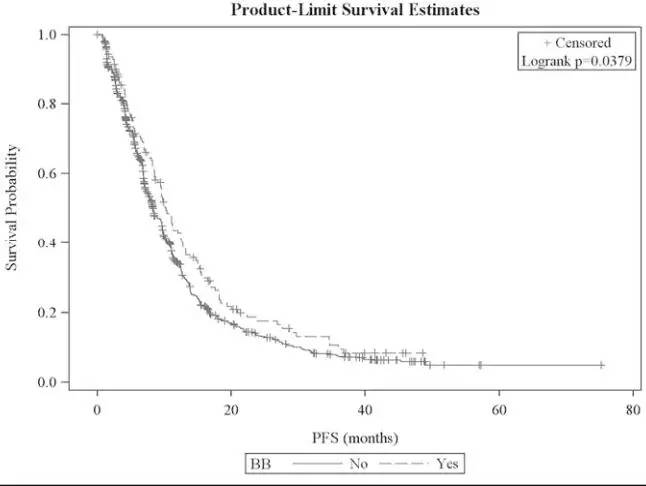
亚型中联合PI3K抑制剂和PARP抑制剂不仅能调节细胞增殖、存活和凋亡,而且能增强BRCA1/2突变的TNBC对PARP抑制剂的敏感性。BELLE-2研究初步结果也已经证实布帕利昔(磷脂酰肌醇-3-羟激酶(PI3K)广泛抑制剂)可以显着改善氟维司群治疗激素受体阳性HER2阴性晚期乳腺癌患者的无进展生存。
邵志敏教授表示,不同亚型独特的基因突变是临床转化研究的指路灯,打破以往三阴性乳腺癌的治疗僵局,有助于医学专家“有的放矢”。邵志敏教授团队根据前期实验结果发明了临床实用的三阴性乳腺癌分子分型方法,结合乳腺外科正在大力推行的精准医学基因检测,可以为每一位患者进行精确的分子分型并鉴定药物靶点,从而有望在临床中实现精准治疗。
根据基础研究数据,他们还提出了“三阴性乳腺癌分子分型基础上的精准治疗策略”。针对这些特殊基因突变研究,结合临床试验,就有机会更早实现临床转化,更快开发出针对不同三阴性乳腺癌靶点的药物,让患者尽早获得精准且能明显提升疗效的治疗方案。未来在精准全程管理理念的指导下,化疗、内分泌、靶向、免疫治疗将可能成为TNBC患者的标准治疗模式。
原始出处:Jiang YZ1, Ma D1, Suo C2, et al. Genomic and Transcriptomic Landscape of Triple-Negative Breast Cancers: Subtypes and Treatment Strategies. Cancer Cell. 2019 Mar 18;35(3):428-440.e5.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阴性乳腺癌#
24
#CEL#
36
#Cell#
28
#cancer cell#
26
#三阴性#
31
#复旦#
26