Nat Commun:脑脊液的免疫细胞分析可表征脑转移瘤微环境
2021-03-11 xiaozeng MedSci原创
脑转移瘤(BrM)是脑部中最常见的肿瘤,是一种破坏性的癌症并发症。
脑转移瘤(BrM)是脑部中最常见的肿瘤,是一种破坏性的癌症并发症。既往研究显示,免疫检查点抑制剂(ICIs,如抗PD1、抗PD-L1、抗CTLA4等)在患有进行性或转移性实体瘤患者中显示出显著的临床益处。然而,仅有一小部分患者对ICI治疗有反应。
免疫细胞浸润的程度和表型已被用于预测对ICI的反应。但是,从脑恶性肿瘤中获取样本具有挑战性,脑肿瘤的解剖位置和相关的外科手术风险也限制了相关免疫表型的表征。
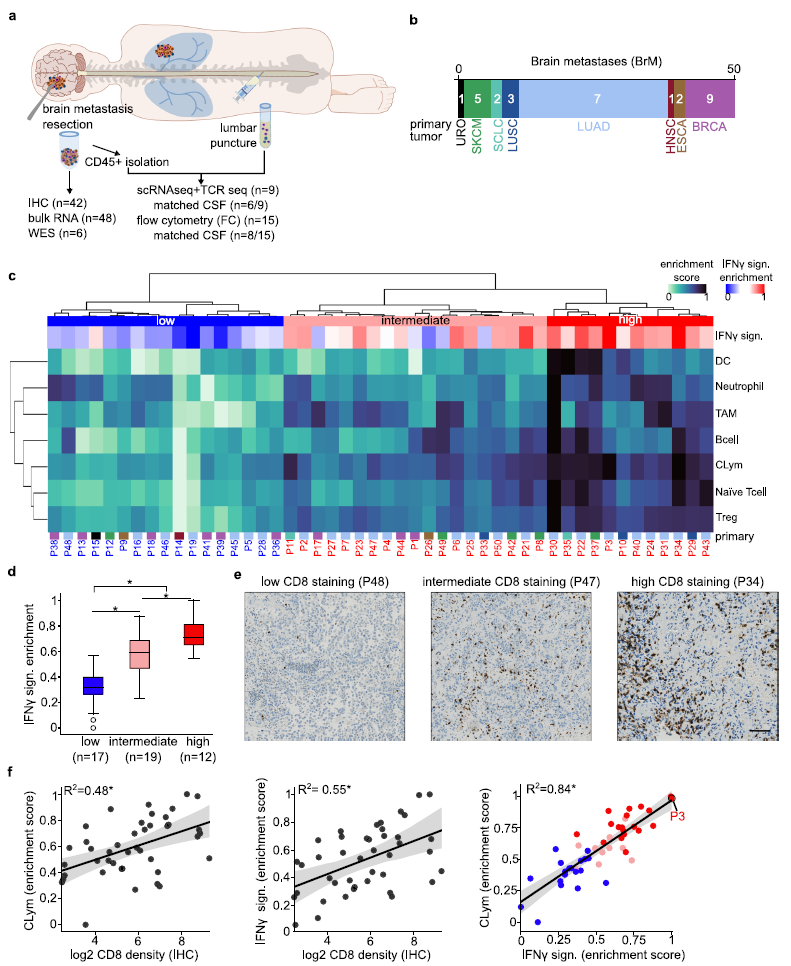
为了全面绘制BrM和对应的脑脊液(CSF)的免疫细胞图谱,在该研究中,研究人员采用了单细胞RNA测序结合T细胞受体基因分型的方式来表征存在于脑部病变和CSF中的免疫细胞。研究人员发现,肿瘤免疫浸润,尤其是CD8+T细胞的浸润可以通过脑脊液的分析来进行辨别,以预测ICI反应的验证状态。同样的,在脑部病变和CSF样本中检测到了相同的克隆型T细胞受体,证实这些区室之间出现了细胞交换。
脑转移瘤中肿瘤免疫浸润模式的鉴定
总而言之,该研究结果揭示,CSF免疫细胞分析可提供一种非侵入性的替代方案,用于预测患者对ICI的反应,并确定脑转移瘤中存在的克隆型T细胞受体。
原始出处:
Rubio-Perez, C., Planas-Rigol, E., Trincado, J.L. et al. Immune cell profiling of the cerebrospinal fluid enables the characterization of the brain metastasis microenvironment. Nat Commun 12, 1503 (08 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
30
#转移瘤#
33
#COMMUN#
32
#脑转移瘤#
57