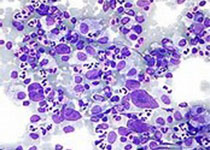
Blood: CD19特异性CAR T细胞疗法治疗R/R B-ALL
2020-01-01 QQY MedSci原创
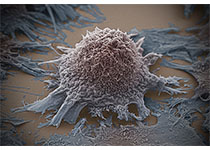
嵌合抗原受体(CAR) T细胞已被证明对复发性/难治性(R/R) 急性B细胞淋巴细胞白血病患者具有临床益处。Curran等人开展了一项多中心的临床试验,检测这种疗法的毒性、可行性和反应性。共招募了25位R/R B-ALL患儿或青年患者(1-22.5岁),予以19-28z CAT T细胞治疗。条件化疗包括高剂量(3 g/m2)环磷酰胺(HD-Cy) 17例,低剂量(≤1.5 g/m2)环磷酰胺(LD
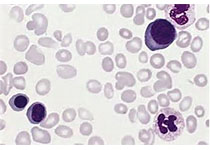
共招募了25位R/R B-ALL患儿或青年患者(1-22.5岁),予以19-28z CAT T细胞治疗。条件化疗包括高剂量(3 g/m2)环磷酰胺(HD-Cy) 17例,低剂量(≤1.5 g/m2)环磷酰胺(LD-Cy) 8例。
15位患者有预处理微小残留病灶(MRD;骨髓原代细胞<5%),10位患者有预处理形态学证据(骨髓原代细胞≥5%)。
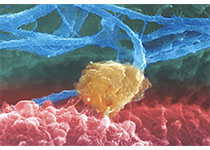
所有毒性作用可逆,包括重度细胞因子释放综合征(16%,4/25)和重度神经毒性(28%,7/25)。所有治疗的患者被纳入反应性分析,在24位可评估的患者中,与没有增加毒性的LD-Cy/形态学组相比,HD-Cy/MRD 队列患者的反应性和CAR T细胞扩增峰值均更佳。
本研究表明CD19特异性CAR T细胞疗法用于R/R B-ALL患者安全性良好。条件化疗的强度和微小预处理病灶负担对反应性有正性效应,且对毒性无副作用。
原始出处:
Kevin J. Curran, et al.Toxicity and response after CD19-specific CAR T-cell therapy in pediatric/young adult relapsed/refractory B-ALL.Blood. December 26, 2019.
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#特异性#
31
#ALL#
29
#CD19#
42
#B-ALL#
56
#T细胞疗法#
29
这是个好消息!
74