Circ Cardiovasc Imaging:左心房重构的影响因素有哪些?
2017-02-20 MedSci MedSci原创
由此可见,人群中左心房扩张在黑人和西班牙裔中比白人个体更常见,并与左心室的平行变化有关。左心房扩张可能是通过血压控制和内脏肥胖的发生所介导。
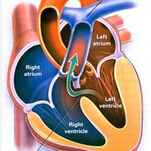
在一般人群中,虽然与左心室重塑的促进因素得到了很好的研究,然而,很少有研究数据描述与左心房(LA)结构变化有关的影响因素。最近,心血管领域权威杂志Circulation-Cardiovascular Imaging上针对这一问题发表了一篇研究文章。
研究人员采用心脏磁共振成像对来自于达拉斯心脏研究中的748名受试者的最大LA体积进行了2次测量,2次测量之间的平均间隔时间为8年。研究人员采用多变量线性回归评估了LA的体积变化(ΔLAV)与传统危险因素、生物学标志物、LV的几何形状、通过心脏磁共振成像评估的重构和整体与局部肥胖的详细测量(通过磁共振成像和双能X线骨密度仪)之间的相关性。
研究人员发现较大的ΔLAV与黑人和西班牙裔的种族/民族、收缩压的变化、左心室质量和Δ左心室质量、N末端脑钠肽前体和N末端脑钠肽前体的变化、体重指数独立相关(所有P<0.05)。在亚组分析中,对ΔLAV与左心室质量参数之间的相关性被基础舒张末期容积和Δ左心室舒张末期容积之间的相关性所驱动(每一个P<0.0001),而与心室壁厚度(P=0.21)无关。对ΔLAV与体重指数的相关性是由内脏脂肪质量相关性进行解释(P=0.002),而ΔLAV和腹部皮下脂肪之间(P=0.47)或低体脂(P=0.30)之间没有观察到相关性。
由此可见,人群中左心房扩张在黑人和西班牙裔中比白人个体更常见,并与左心室的平行变化有关。左心房扩张可能是通过血压控制和内脏肥胖的发生所介导。
原始出处:
Walter Oliver,et al. Factors Associated With Left Atrial Remodeling in the General Population. Circ Cardiovasc Imaging. 2017. https://doi.org/10.1161/CIRCIMAGING.116.00504
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#左心房#
48
#ASC#
37
#影响因素#
31
#心房#
36
这个很不错
64