Eur J Nucl Med Mol Imaging:[18F]DCFPyL PET/CT对前列腺癌切除术后低PSA水平的复发转移的诊断和定位价值
2021-01-09 Nebula MedSci原创
前列腺癌(Prostate cancer,PC)是最常见的癌症之一。可治愈前列腺癌患者的标准治疗方法是根治性前列腺切除术(RP)或放疗;然而,超过1/3的患者会复发。本研究是一项回顾性的多中心分析,旨
前列腺癌(Prostate cancer,PC)是最常见的癌症之一。可治愈前列腺癌患者的标准治疗方法是根治性前列腺切除术(RP)或放疗;然而,超过1/3的患者会复发。本研究是一项回顾性的多中心分析,旨在评价采用[18F]DCFPyL的前列腺特异性膜抗原(PSMA)PET/CT在诊断和定位前列腺癌根治术(RP)后复发中的作用。特别提到PSA0.5 ng/mL以下的低PSA组,以帮助围绕将这一组纳入指南和筹资途径的讨论。
对澳大利亚和新西兰的PSMA联合数据库患者进行回顾性分析。222例RP术后复发患者被分成5个PSA组(ng/mL):0~0.19、0.2~0.49、0.5~0.99、1~1.99和≥2。[18F]DCFPyLPET/CT检查发现的病灶被记录为局部复发、区域淋巴结和转移。
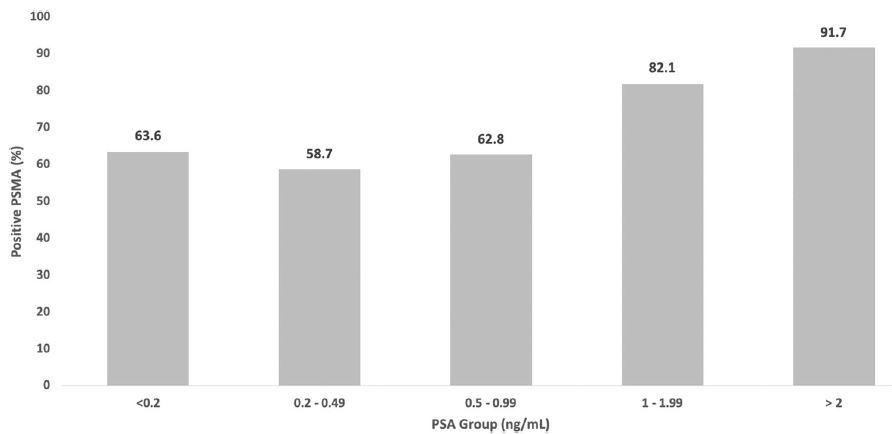
[18F]DCFPyL PET/CT在不同PSA水平组的复发检出率
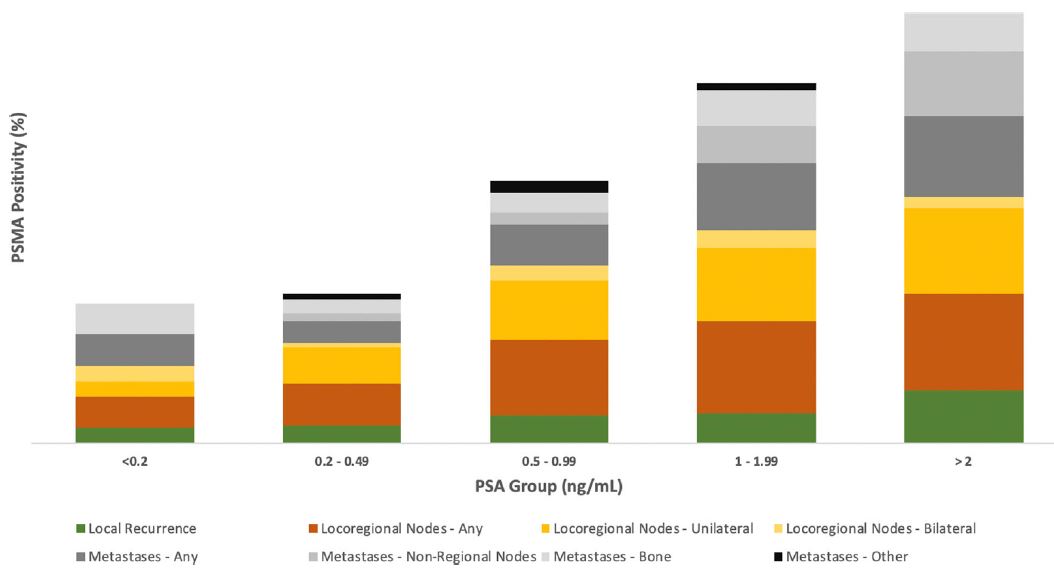
不同PSA水平组PSMA的表达水平
在222例患者中,155例(69.8%)有摄取异常,提示前列腺癌复发。[18F]DCFPyLPET/CT检查对PSA水平在≥2 ng/mL、1~1.99 ng/mL、0.5~0.99 ng/mL、0.2~0.49 ng/mL、≤0.2 ng/mL的患者的诊断效率分别为91.7%(44/48)、82.1%(23/28)、62.8%(27/43)、58.7%(54/92)、63.6%(7/11)。
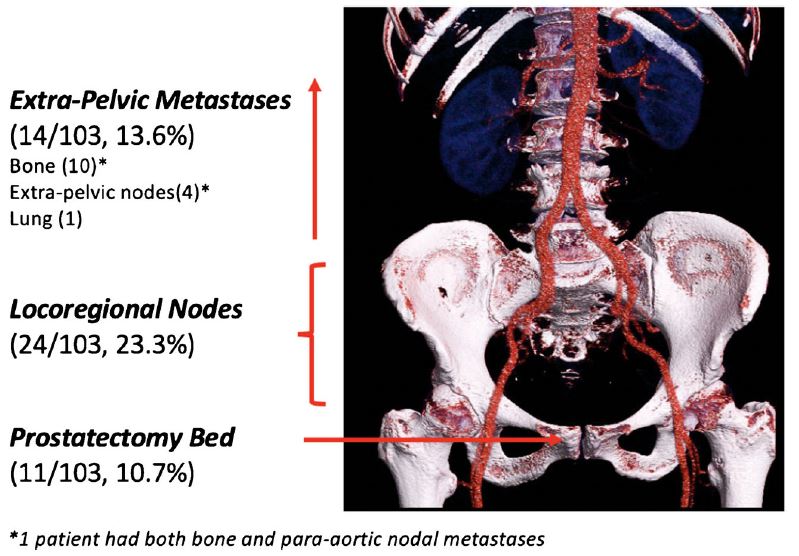
PSA<0.5 ng/mL的患者的复发部位
在PSA<0.5 ng/mL的患者中,47.6%(49/10 3)的患者可检出病变,71.4%(35/49)的病变局限于盆腔,22.4%(11/49)的为前列腺床复发,49.0%(24/49)的有盆腔淋巴结转移,28.6%(14/49)的有盆腔外病变。
综上所述,[18F]DCFPyL PET/CT对RP术后复发病例的检出率较高,即使在PSA值较低时(PSA值低于0.5 ng/mL时复发患者的检出率基本保持不变)。在确定PSMA PET/CT资助资格指南时使用严格的PSA阈值可能会导致大量低于此类阈值的患者因不能及时确诊而耽误治疗。
原始出处:
Perry, E., Talwar, A., Taubman, K. et al. [18F]DCFPyL PET/CT in detection and localization of recurrent prostate cancer following prostatectomy including low PSA <0.5 ng/mL. Eur J Nucl Med Mol Imaging (2021). https://doi.org/10.1007/s00259-020-05143-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
36
#切除术#
37
#DCF#
38
#PSA#
37
#PET/CT#
60
#PET#
33
#Med#
25
前列腺癌相关研究,学习了,谢谢梅斯
54
#前列腺癌 切除术 随访#
69
#前列腺癌#
171