J Clin Oncol:中科院&协和:术前短程放疗+化疗方案或可替代局部晚期直肠癌的标准长程放化疗方案!
2022-03-10 Nebula MedSci原创
术前短程放疗+化疗方案或可替代局部晚期直肠癌的标准长程放化疗方案
长期同步放化疗(CRT)后继以全直肠系膜切除术(TME)是局部晚期直肠癌(LARC)的一线治疗方案。此外,有大约 50% 的患者在CRT和手术后会接受辅助化疗。
本研究旨在明确,对于局部晚期直肠癌患者,术前短期放疗后化疗的效果是否不逊于标准长期放化疗方案。
这是一项由北京协和与中国医学科学院设计的在中国开展的多中心、随机的3期临床试验,招募了位于直肠远端或中三分之一的3-4期的和(或)区域淋巴结阳性的临床原发性直肠癌患者,随机(1:1)分成两组,接受短期放疗(一周内25Gy,分5次)继以四个疗程的化疗(全新辅助治疗[TNT])或同步放化疗(CRT)(5周内50Gy,分25次,同步卡培他滨化疗)。术前治疗后 6-8 周进行全直肠系膜切除术。术后TNT组和CRT组分别继续接受两个和六个疗程的CAPOX化疗。主要终点是3年无病生存率(DFS)。
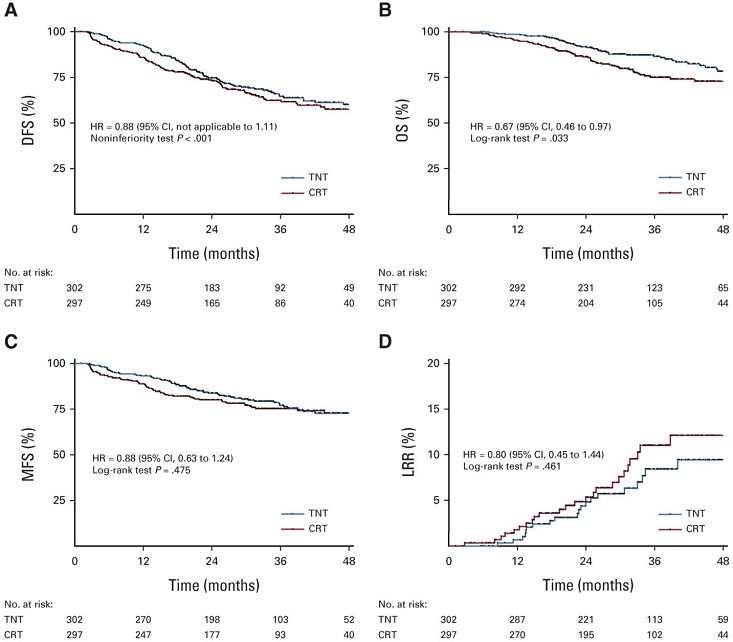
两组患者的存活预后
2015年8月至2018年8月期间,共599位患者被随机分至TNT组(n=302)或CRT组(n=297)。中位随访了35.0个月后,TNT组和CRT组的3年DFS分别是64.5%和62.3%(风险比[HR] 0.883,p<0.001)。两组的无转移生存率和局部复发率均无明显差异,但TNT组的3年总生存率优于CRT组(86.5% vs 75.1%,p=0.033)。
此外,无论预后因素如何,两种治疗对DFS和总生存率的影响相近。术前治疗期间,TNT组和CRT组的III-V级的急性毒性事件的发生率分别是26.5%和12.6%(p<0.001)。
综上,对于局部晚期直肠癌患者,术前进行短期放疗+化疗的方案是有效的,且毒性可接受,可作为标准长程放化疗方案的替代方案。
原始出处:
Jing Jin, et al. Multicenter, Randomized, Phase III Trial of Short-Term Radiotherapy Plus Chemotherapy Versus Long-Term Chemoradiotherapy in Locally Advanced Rectal Cancer (STELLAR). Journal of Clinical Oncology. March 9, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.01667
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
26
#中科院#
50
#局部晚期#
28
#局部晚期直肠癌#
40
#放化疗#
48
#协和#
41
#局部#
28