Br J Cancer:III期临床试验:选择性淋巴结照射和或厄洛替尼联合放化疗改善局部晚期食道鳞状细胞癌患者长期生存率
2020-09-24 xiaozeng MedSci原创
食道癌作为全球癌症相关死亡的最常见原因之一,放化疗(CRT)同步使用目前被认为是局部晚期食道鳞状细胞癌(ESCC)患者的标准治疗策略。在RTOG 8501临床试验中,相比于单独放疗,5-氟尿嘧啶结合顺
食道癌作为全球癌症相关死亡的最常见原因之一,放化疗(CRT)同步使用目前被认为是局部晚期食道鳞状细胞癌(ESCC)患者的标准治疗策略。在RTOG 8501临床试验中,相比于单独放疗,5-氟尿嘧啶结合顺铂的放化疗治疗能够显著改善患者的5年总生存率。然而,患者的长期治疗结果仍令人沮丧,局部复发率超过50%。因此,急需进一步的改善治疗策略并寻找更有效的药物,以改善这些患者的预后。
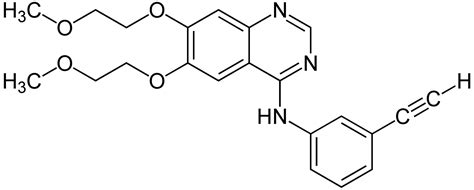
该研究旨在评估两个假设的III期临床研究的长期结果:在ESCC患者中,(1)选择性淋巴结照射(ENI)效果优于常规射线野照射(CFI);(2)局部放化疗联合厄洛替尼(erlotinib)效果优于单独的局部放化疗。
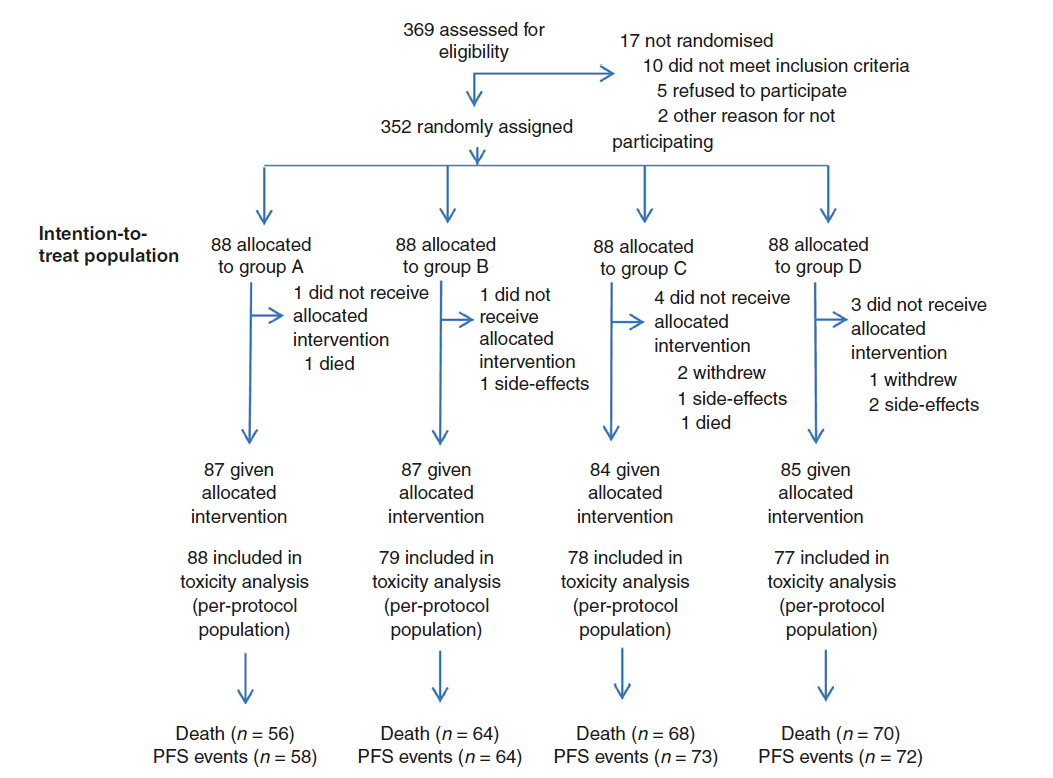
研究流程图
研究人员将局部晚期ESCC患者随机分配到四个治疗组中:A组:ENI放疗结合两个周期的TP(紫杉醇和顺铂)联合厄洛替尼治疗;B组:ENI放疗结合两个周期TP化疗;C组:CFI放疗结合两个周期的TP联合厄洛替尼治疗;D组:CFI放疗结合两个周期TP化疗。并探讨EGFR(表皮生长因子受体)的表达对厄洛替尼联合放化疗疗效的影响。
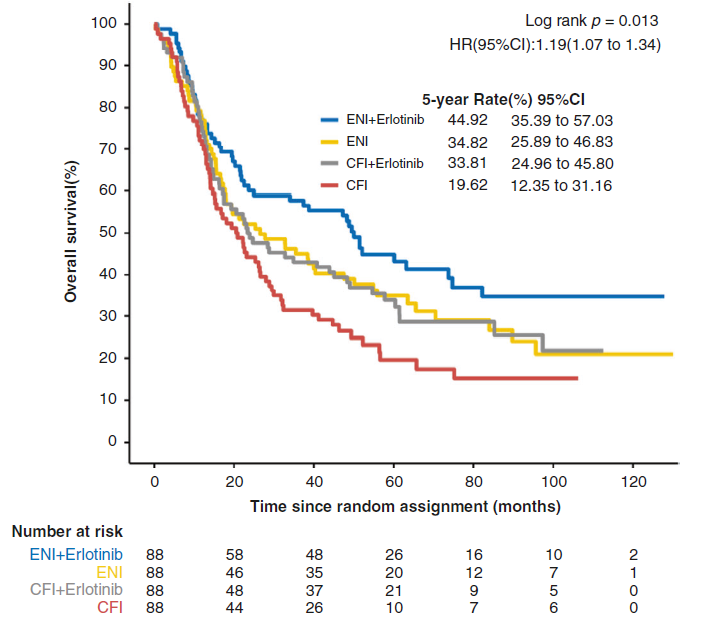
4个治疗组的Kaplan-Meier生存分析
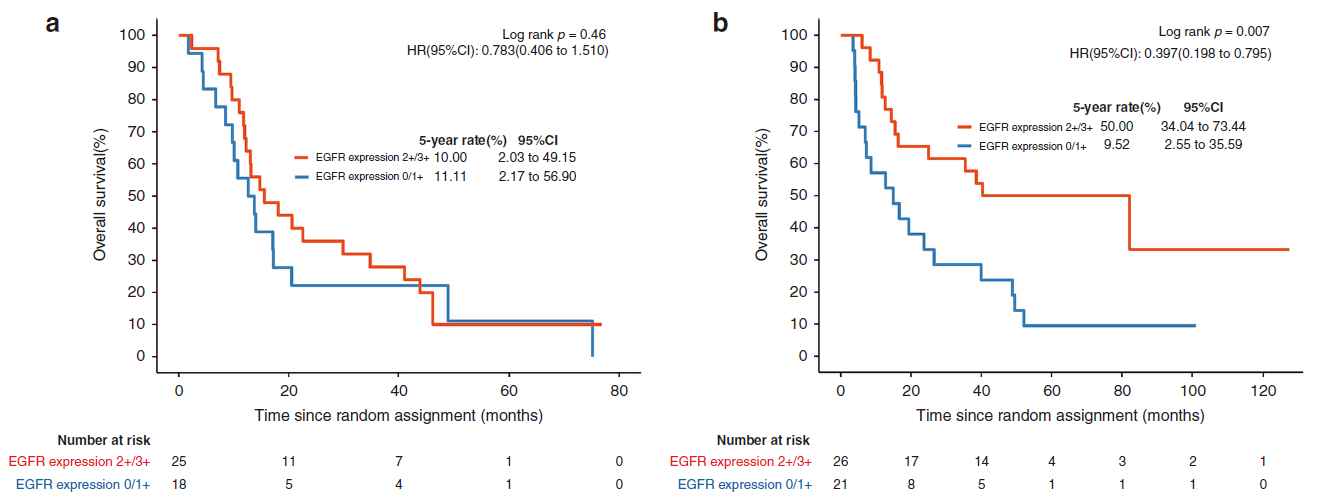
该研究共募集352名患者(每个治疗组88名患者)入组。结果显示:A,B,C,D四个组的5年生存率分别为44.9%,34.8%,33.8%和19.6%。与标准CFI相比,ENI能够显著改善患者的总生存期(OS)(中位时间为38.5对22.6个月)。厄洛替尼联合治疗同样能够显著改善患者的OS(中位时间39.4对27.4个月)。进一步研究显示,在EGFR过表达的患者中,厄洛替尼联合治疗相比于对照组患者具有更好的OS和无进展生存期(PFS)。
EGFR表达状态对患者生存期的影响
综上,该研究结果显示,选择性淋巴结照射和/或厄洛替尼联合放化疗可以改善局部晚期食道鳞状细胞癌患者的长期生存率。
原始出处:
Xie, C., Jing, Z., Luo, H. et al. Chemoradiotherapy with extended nodal irradiation and/or erlotinib in locally advanced oesophageal squamous cell cancer: long-term update of a randomised phase 3 trial. Br J Cancer (22 September 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#III#
34
#I期临床#
30
#I期临床试验#
45
#局部晚期#
19
#细胞癌#
25
#II期临床试验#
22
#选择性#
28
#III期#
31
#长期生存#
25
#III期临床试验#
22