CGH:自膨式金属支架治疗恶性远端胆道狭窄的效果优于塑料支架
2022-01-26 MedSci原创 MedSci原创
胆管狭窄是由于胆管损伤和复发性胆管炎所致或是先天性而导致的胆管腔瘢痕性缩窄。胆管狭窄可由医源性损伤、腹部外伤和胆囊结石、胆管结石、胆管炎症等刺激,导致胆管壁纤维组织增生、管壁变厚、胆管内腔逐渐缩窄。
目前在临床工作中,内镜下放置支架是缓解恶性胆道梗阻的首选疗法。其中,与经皮引流相比,内窥镜逆行胰胆管造影(ERCP)引导下的塑料支架(PS)手术提供了一种有效的、侵入性较低的胆管减压方法。随后有研究人员开发了自膨式金属支架(SEMS),并证实比PS有更持久的治疗反应,但是SEMS更容易出现组织增生,导致胆管重新闭合。此外,PS的治疗成功率与SEMS的治疗成功率相当,但费用却高得多。因此,本项研究旨在比较SEMS和PS在治疗恶性胆管狭窄方面的疗效差异。

研究人员对所有接受ERCP支架置入治疗恶性胆管狭窄的连续患者进行了一项回顾性队列研究。然后对临床治疗成功率、通畅持续时间、支架功能障碍、计划外再干预和不良结果进行了统计学比较。最后进行单变量和多变量分析以筛选与临床成功、再次干预的需要和支架功能障碍相关的因素。
本项研究发现从 2012 年到 2019 年,共有1139 名患者接受了 ERCP 和 PS 放置手术,1008名患者接受了 SEMS 治疗恶性胆管狭窄。在远端狭窄方面,SEMS 报告的临床成功率显着高于 PS(94.1% VS 87.4%,P < 0.001),并且有较低的计划外再干预率(17.1% VS 27.4%,P< 0.001)。在胆管狭窄中,临床成功率和计划外干预率相当。无论狭窄位置如何,SEMS 的通畅持续时间和非计划再干预时间明显长于 PS。在远端狭窄中,PS 与胆管炎的发生率显着高于 SEMS(6.9% VS 2.4%;P<.001),但胰腺炎的发生率较低(3.6% VS 6%;P=0.021)。
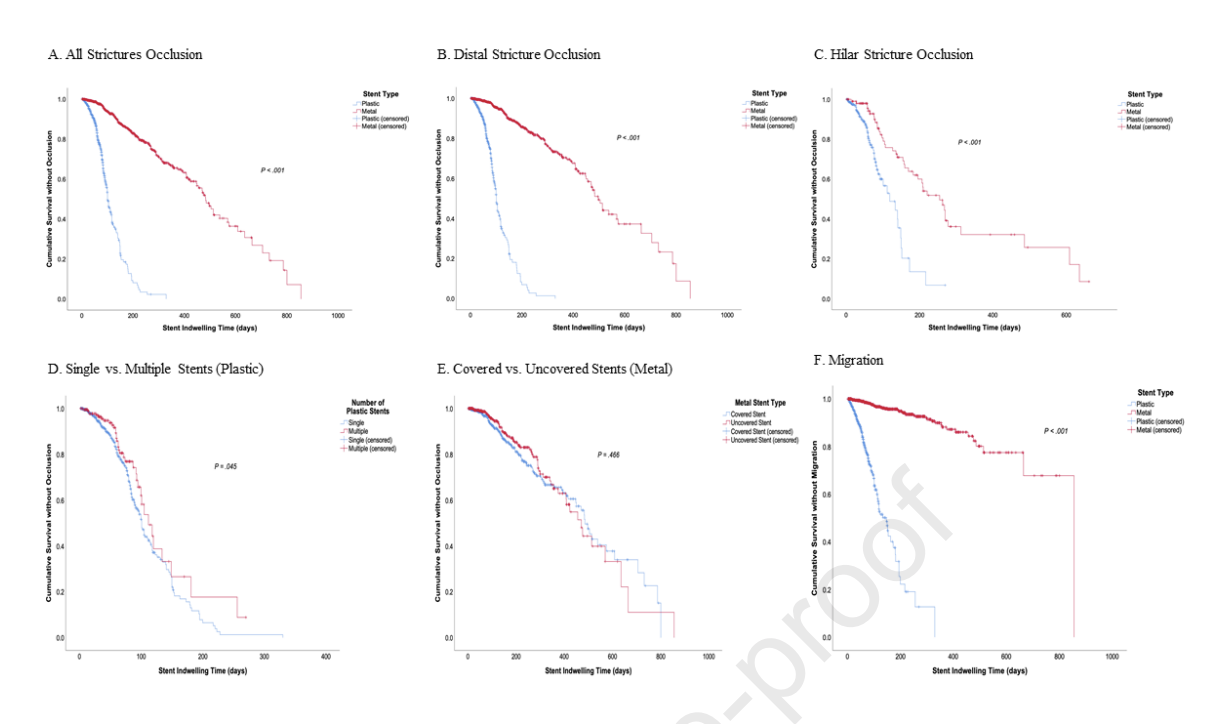
图:胆管狭窄预后情况
本项研究结果证实鉴于卓越的疗效、持久性和较低的胆管炎发生率,SEMS 应作为恶性远端胆道狭窄的一线内镜治疗选择。对于恶性胆管狭窄,SEMS 在某些情况下是 PS 的替代品,因为它提供了相当的功效和卓越的耐用性。
原始出处:
Sunguk Jang. Et al. Superiority of Self-Expandable Metallic Stents Over Plastic Stents in Treatment of Malignant Distal Biliary Strictures. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#金属支架#
36
#CGH#
36
#支架治疗#
45
好文章
55
好文章,谢谢分享。
66