ASCO 2022:胃肠道肿瘤领域重磅研究进展
2022-06-05 MedSci原创 MedSci原创
2021年6月4日,全球肿瘤界的年度盛会——美国临床肿瘤学会(ASCO)年会正式拉开序幕,国内外诸多顶级研究成果即将公布。梅斯医学将持续关注并报道学术亮点,分享给各位同道。
2021年6月4日,全球肿瘤界的年度盛会——美国临床肿瘤学会(ASCO)年会正式拉开序幕,国内外诸多顶级研究成果即将公布。梅斯医学将持续关注并报道学术亮点,分享给各位同道。

本文梅斯医学为大家整理了胃肠道肿瘤国内外重磅研究,分享给各位同道。
1、晚期胰腺导管腺癌的长期和短期幸存者的分子特征
由于缺少有效的筛查手段和早期诊断方法,大多数患者为局部晚期及转移性胰腺导管腺癌(PDAC),而晚期PDAC患者的中位总生存期为1年以下。
有研究显示,虽然晚期PDAC患者的预后仍不理想,但相比未治疗者,接受化疗的患者中位总生存期可延长约2倍。有些患者则病情发展迅速,这也意味着PDAC生物学异质性。因此,了解PDAC的生物学差异,显得至关重要。
研究人员从COMPASS(NCT02750657)和POG/PanGen(NCT02155621,NCT02869802)研究中收集了诊断为局部晚期或转移性 PDAC 的患者的电子病历,患者的ECOG PS为0-1,化疗方案基于临床医生的偏好,并采用 HRDetect 测定法鉴定同源重组缺陷。研究人员比较了极短总生存期(STS)(≤3 个月)和长总生存期(LTS)(≥24个月)患者的生物学特征。
结果显示,341 例患者被纳入分析,其中 47 例为 STS(mOS 1.6 个月)和 42 例 LTS(mOS 29.7 个月)。队列之间的中位年龄、BMI 或性别没有差异。STS更有可能在诊断时有ECOG PS 1 vs 0,更高的肿瘤负担(RECIST)和更高的CA19.9。
在 STS 中,71% 的患者在首次扫描前因临床下降或死亡而出现无法评估的反应,28% 的 PD 为最佳反应。在LTS中,化疗的ORR为69%。64%和33%的LTS以及32%和36%的STS分别接受了mFFX和GA。KRAS突变(90% vs 98%)或特定突变等位基因的发生率没有差异,但是突变KRAS的扩增在 STS 中更常见(35% vs 65%,p=0.01)。
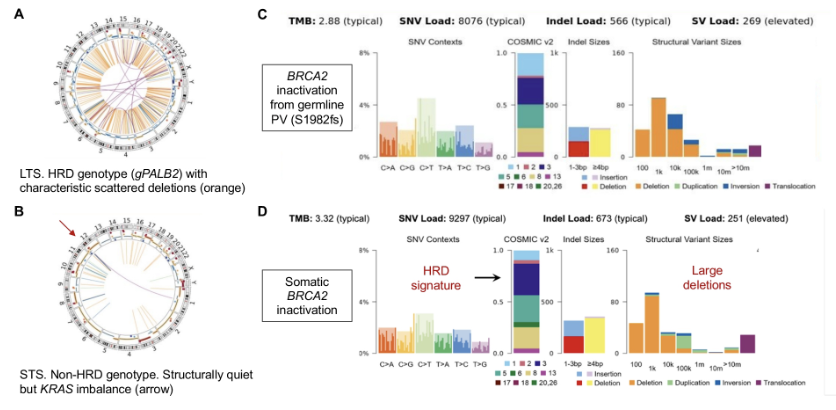
TP53、CDKN2A和SMAD4(90% vs 98%)以及参与染色质修饰的基因(ARID1A、SMARCA4、PBRM1、KDM6A)的失活驱动突变(17% vs 30%,无)的发生率在两组中相似。然而,STS 的突变发生率较高,导致 PI3K/AKT/mTOR 通路激活。然而,在 LTS 中,6/7 是种系致病变异的结果,而在 STS 中只有 1/5。肿瘤结构变异负荷、TMB 和替换碱基特征在两个队列中相似。
总之,晚期PDAC患者生存期≤3个月,其特点是肿瘤负担较重,分子谱与增强的 RAS 信号传导一致、PI3K/AKT/mTOR途径失调和基底类转录组亚型。HRD基因是异质性的,LTS携带了部分HRD基因。
2、ctDNA检测能更早发现胃癌的复发风险
循环肿瘤 DNA (ctDNA)是血液中肿瘤衍生的片段化DNA,是一种具有特征性的肿瘤标志物。通过ctDNA的相关检测,可以检测到肿瘤在患者血液中的踪迹信息。目前,ctDNA检测已成为包括胃癌患者在内的各种肿瘤类型的潜在预后标志物。
研究人员招募了来自2016年10月至2019年6月100 名 II/III 期可切除胃癌患者(NCT02887612)。在围手术期和辅助化疗 (ACT) 后收集原发性肿瘤和血浆样本。通过 425 个癌症相关基因的靶向测序来捕获体细胞变异。只有当在血浆中检测到一种或多种变异出现在至少2%的原发性肿瘤中时,患者的血浆才被定义为 ctDNA 阳性。所有患者均接受了标准护理治疗。
结果显示,术前,38 名患者血浆中可检测到ctDNA,但其预测复发的价值有限。术后,25 名患者的血浆 ctDNA 仍呈阳性,且复发风险高于非阳性患者。41 名患者在辅助化疗后,对其血浆进行评估,其中10名ctDNA 阳性患者的复发和死亡风险明显高于 ctDNA 阴性患者。
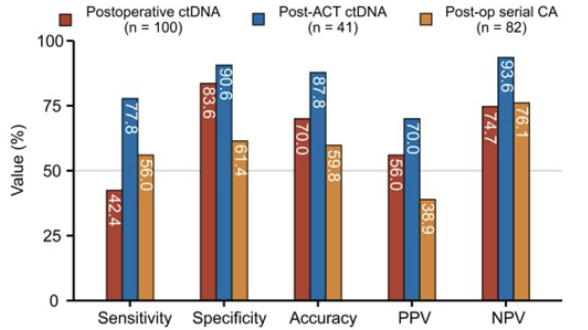
特别是,与术后ctDNA和治疗后肿瘤生物标志物,即CEA、CA199和CA72-4相比,辅助化疗后 ctDNA 获得了更好的预测性能,敏感性为 77.8%,特异性为 90.6%。在所有多变量分析中,ctDNA 阳性是 RFS 的独立因素。与 ERBB4 野生型患者相比,原发性肿瘤中存在 ERBB4 突变的患者 RFS 较差。因此,术后和辅助化疗后,ctDNA 与 II/III 期胃癌患者残余病灶和高复发风险相关,或可用于指导术后胃癌患者管理。
3、真实世界研究:低剂量阿帕替尼治疗晚期肝细胞癌的疗效和安全性
阿帕替尼是一种酪氨酸激酶抑制剂,通过高度选择性竞争细胞内VEGFR-2的ATP结合位点,抑制酪氨酸激酶的生成从而抑制肿瘤组织新血管的生成,从而达到抗肿瘤目的。有研究显示,阿帕替尼对晚期肝细胞癌 (HCC) 的良好的疗效。然而,在真实世界中,阿帕替尼的有效性和安全性还有待研究。因此,本研究旨在揭示现实世界中低剂量阿帕替尼治疗晚期HCC的疗效和安全性。
2017 年 1 月至 2020 年 8 月期间,研究人员纳入了在三个不同机构接受阿帕替尼治疗的 178 名晚期 HCC 患者。
174名患者每天接受口服阿帕替尼250毫克,4名患者每天接受500毫克,直到疾病进展。25 名和 103 名患者还分别接受了至少一次免疫治疗和经导管动脉化疗栓塞 (TACE) 治疗。肿瘤反应和不良反应分别按照RECIST 1.1和CTCAE 5.0进行评价。使用 Kaplan-Meier 方法分析生存曲线。Cox 比例风险模型用于确定单变量和多变量的预后价值。
结果显示,随访24个月,患者达到完全缓解(CR)、部分缓解(PR)、疾病稳定(SD) 和进行性疾病 (PR)分别有 0(0%)、28(15.73%)、103(57.87%)和 47(26.40%),总体缓解率(ORR)和疾病控制率(DCR)分别为15.73%和73.60%。有趣的是,28 例PR患者中,27 例接受阿帕替尼作为一线或二线治疗,21 例接受免疫治疗或 TACE 作为联合治疗,表明早期应用阿帕替尼联合治疗可以提供更好的疗效。

另外,Kaplan-Meier 分析显示,中位总生存期 (OS) 和无进展生存期 (PFS) 分别为 16.0 个月和 7.0 个月。三线治疗和PVTT与较差的PFS独立相关。相反,阿帕替尼联合免疫疗法或与更好的PFS独立相关,也有更好的OS。在不良反应方面,最常见的治疗相关不良事件为高血压(29.21%)、疲劳(16.85%)、手足综合征(16.29%)、呕吐(14.04%)、肝功能障碍(6.18%)和蛋白尿(6.74%)。未观察到严重(≥3 级)不良事件。
总之,低剂量阿帕替尼能够为晚期HCC提供有效和安全的治疗,同时早期应用阿帕替尼和联合治疗可以提供更好的疗效。
4、晚期胃癌和食管癌患者四种临床预后评分的比较
尽管有几个临床评分系统可以帮助肿瘤学临床试验的进行预后评估,但并没有统一的标准。本研究比较了四种预后评分对晚期胃癌和食道癌(GE)患者总生存期(OS)的预测能力。
该研究纳入了来自2007年至2020年年间加拿大玛格丽特公主癌症中心接受一线姑息性系统治疗的晚期(不可切除或转移)GE癌症患者,并使用四个评分系统确定了高预后风险的患者。皇家马斯登医院评分(RMH)、MD安德森癌症中心评分(MDACC)、Gustave Roussy免疫评分(GRIm-S)和MD安德森免疫检查点抑制剂(MDA-ICI)评分。
结果显示,共纳入451名晚期GE癌症患者,中位年龄为59岁,68%为男性,51%为ECOG状态0-1,63%表现为新发转移性疾病。通过四种评分,被归类为高风险的患者比例为:RMH 25%(N=113),MDACC 13%(N=95),GRIm-S 24%(N=109),MDA-ICI 26%(N=117)。在所有评分系统中,高风险患者的OS明显较短。(中位 OS 7.9 vs 12.2 个月,RMH 高风险 vs 低风险,p<0.001;MDACC 6.8 vs. 11.9 个月 p<0.001;5.3 vs. 13 个月 p<0.001对于 GRIm-S;8.2 与 12.2 个月,对于 MDA-ICI,p<0.001)。
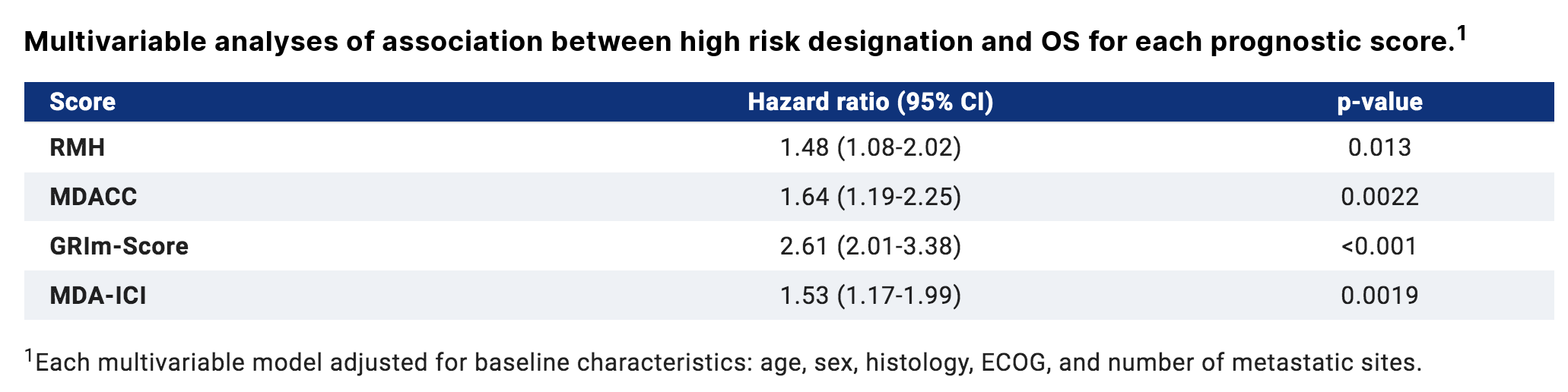
在多变量分析中,每个预后评分都与 OS 显著相关。GRIm-S 具有最高的预测辨别力和最高的早期死亡预测能力。
综上,所比较的四个预后评分系统在预测晚期GE癌患者的OS方面都有合理的准确性。预测早期死亡的较高准确性可能首选GRIm-S评分。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肠道肿瘤#
40
#肿瘤领域#
42
#ASC#
48
#胃肠道#
51
#研究进展#
50
#胃肠道肿瘤#
61
#重磅#
47