胸腹盆会阴部皮下钢筋贯通伤1例
2018-11-17 黄松庭 临床骨科杂志
患者,男,45岁,因左侧胸腹盆会阴部钢筋贯通伤2h急诊转入我科。患者2h前由2m多高处坠落,1根生锈的钢筋经左侧阴囊,途经左侧腹股沟、左侧盆部、腹部,穿通于左侧胸部乳头平面。受伤整个过程中患者神志清楚,诉伤口疼痛。心电监护示:心率120次,血氧饱和度100%,呼吸20次,血压19.68/9.31kPa。查体:腹软,无肌紧张及反跳痛,左侧腹及左胸壁可见钢筋贯通形状,会阴部钢筋残端外露65CM,见图1
患者,男,45岁,因左侧胸腹盆会阴部钢筋贯通伤2h急诊转入我科。患者2h前由2m多高处坠落,1根生锈的钢筋经左侧阴囊,途经左侧腹股沟、左侧盆部、腹部,穿通于左侧胸部乳头平面。受伤整个过程中患者神志清楚,诉伤口疼痛。心电监护示:心率120次,血氧饱和度100%,呼吸20次,血压19.68/9.31kPa。查体:腹软,无肌紧张及反跳痛,左侧腹及左胸壁可见钢筋贯通形状,会阴部钢筋残端外露65CM,见图1A。
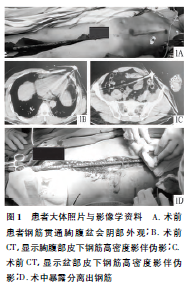
CT检查:肺部及双侧肋骨未见明显异常,左侧腹股沟区、阴囊至前胸腹壁皮下损伤,见图1B、C。骨科、泌尿外科、普外科及胸外科4组医师协同抢救,并立即联合手术治疗。全身麻醉后常规消毒铺巾,沿钢筋走形方向做一65CM的长切口,依次切开皮肤及皮下部分脂肪组织,暴露皮下整个钢筋,见图1D。取出钢筋,使用1%稀释活力碘、医用双氧水及生理盐水冲洗伤口数次,清除残留的异物及铁屑,清除挫伤变性的脂肪组织,严密止血,阴囊会阴部伤口一期缝合,胸腹盆部伤口使用VSD材料覆盖创口。术后使用抗生素治疗3d,术后第3天行清创+VSD术,术后第6天行清创缝合术。2周后拆线,伤口愈合良好,局部无红肿及渗液,住院21d出院。术后测量钢筋全长130CM,血染65CM,钢筋直径2.0CM。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#会阴部#
50
#贯通伤#
49
#会阴#
45