Photoacoustics:通过光声光谱学和机器学习结合有益于诊断前列腺癌
2021-06-16 MedSci原创 MedSci原创
最近,Photoacoustics杂志发文描述了机器学习方法的应用(包括无监督层次聚类和监督分类)诊断前列腺癌的光声频谱分析。
前列腺癌是一种发病率高、转移后治愈率低的疾病。根据2019年的癌症统计数据,前列腺癌是全球男性中第二大最常见的癌症(仅次于肺癌和支气管癌)。前列腺癌最常用的医学影像诊断技术,如超声或磁共振成像(MRI),无法提供化学成分信息,分辨率差,成本高。因此,满足前列腺癌诊断的高准确性、高灵敏度、低侵袭性的标准仍然是困难的。
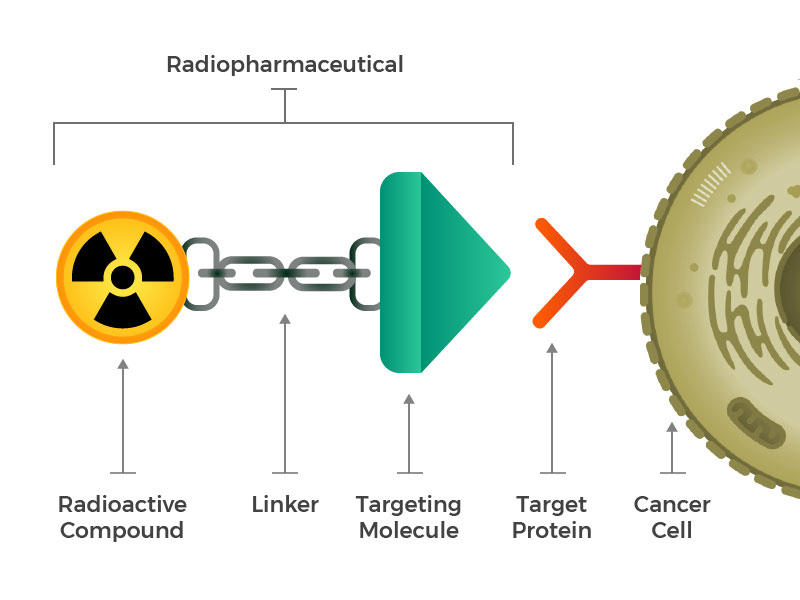
光声理化分析(PAPCA)在前列腺癌的诊断中显示出巨大的潜力。由于分子键和振动模式的差异,不同的生物大分子具有独特的光吸收光谱,可以在不同的光照下检测到。同时,利用光声信号的超声功率谱也可以根据生物组织的声学特性进行表征。由于其超声和光学特性,该方法可以同时评估前列腺组织的化学成分和显微组织学特征,具有高分辨率和灵敏度,且微创。这一领域的进展将需要解决现有成像技术在前列腺癌诊断中的局限性,探索病理检测和分析,并开发诊断工具。
光声光谱技术可以产生丰富的生物组织的化学和物理信息。然而,如此丰富的信息使得直接比较这些组织变得困难。数据挖掘方法可以避开这个问题。
最近,Photoacoustics杂志发文描述了机器学习方法的应用(包括无监督层次聚类和监督分类)诊断前列腺癌的光声频谱分析。

该研究将PAPCA与机器学习相结合,分析前列腺癌演变对应的光声理化谱的特征变化。旨在阐明基于光声理化谱的前列腺癌诊断的可行性。
从22例根治性前列腺切除术中获得101例标本。然后,基于无监督聚类对正常和肿瘤前列腺组织不同波长的功率谱进行相关性分析。首先,旨在探讨不同生物大分子在前列腺癌进化过程中的微观结构分布变化。第二,阐明基于光声理化谱实现前列腺癌诊断的可行性。随后,基于监督线性判别分析(LDA)和二次判别分析(QDA)算法,对光声理化谱进行降维和特征参数提取,用于前列腺癌的诊断。
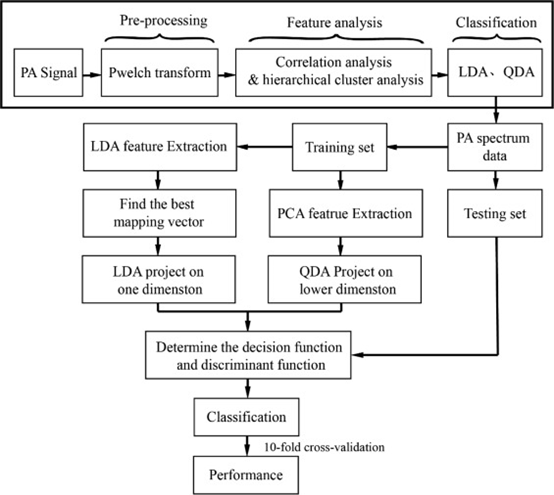
机器学习算法框图
该研究关注的是血红蛋白、胶原蛋白和脂质的含量和分布,因为这些分子在前列腺癌的发展过程中会发生变化。
典型的正常和肿瘤组织的光声理化谱如下图所示。光谱显示了正常组织和肿瘤组织之间的差异。在这两个区域,肿瘤组织的光声理化信号都比正常组织(橙色虚线框)强得多。在690-950 nm波段,主要的光和声源是血红蛋白。这条带内肿瘤组织的颜色明显强于正常组织,因为肿瘤进化过程中血管的增殖增加了肿瘤组织的整体血红蛋白含量。在1200-1370 nm波段,主要的光声源是脂质和胶原蛋白。它们的信号也显著增强,表明前列腺组织的脂质和胶原蛋白含量在癌变过程中增加。将光声信号强度谱(图3b)与不同生物分子的光吸收谱(图3c)进行比较,可以更清楚地观察到这两个区域的信号增强。
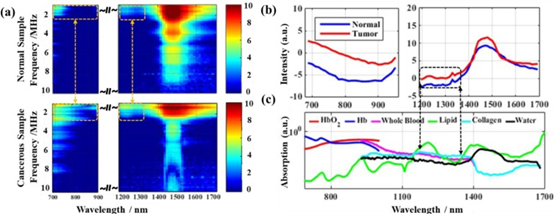
上图所示为癌变样本与正常样本的光声理化谱比较。(a)典型正常(上)和癌(下)的光声理化光谱。(b)正常和癌变样本的光吸收光谱。正常前列腺组织和癌变前列腺组织在胶原蛋白和脂质吸收方面的差异如图黑盒子所示。(c)生物组织中主要分子组分的相对光吸收光谱。
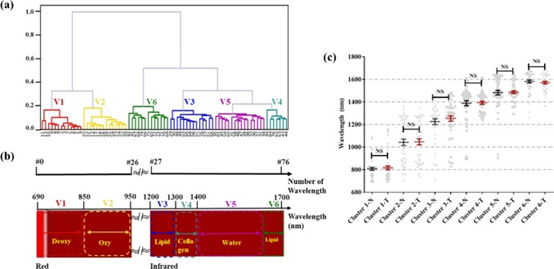
聚类分析的有效性。(a) UPGMA结果的典型聚类树。(b)生物大分子的光吸收光谱及波长编号示意图。(c)正常和癌变样本的统计聚类结果。
使用PCCs和UPGMA将77个波长聚为6个波长组(图4a)。将聚类结果与生物分子的光吸收光谱进行比较(图4b)。虽然聚类树的77个终端节点不是按0-76的顺序排列,但图4a中的波长分组与图4b中不同生物大分子的光吸收基团高度一致。此外,由于分子键和振动模式的不同,不同生物大分子具有独特的光吸收光谱。UPGMA有助于分析光声光谱的差异,确定不同生物大分子产生的光声信号占主导地位的检测波长范围。由于正常组织和癌组织中的主要生物分子没有变化,所以正常组织和癌组织的聚类结果没有显著性差异。
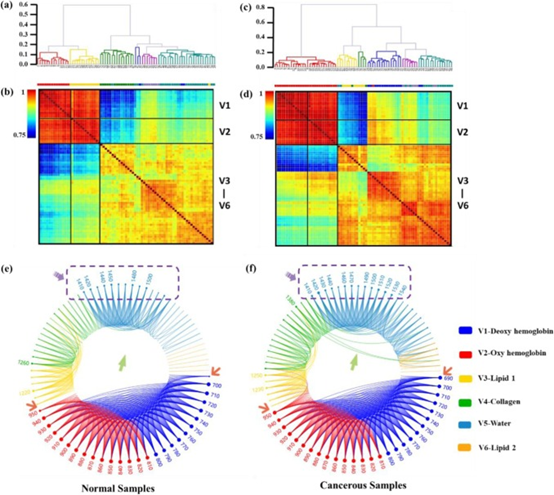
比较正常和癌变样本的相关性。(a)正常样本的聚类树。(b)正常样本热图。(c)癌变样本的聚类树。(d) 癌变样本热图。(e)正常群体的相关权重(WR)网络图。(f)肿瘤组WR网络图。请注意链接(绿色箭头)和标签(紫色箭头)的数量增加,以及较大的节点(橙色箭头)。

传统的基于信号处理的方法和基于机器学习的方法的对比图
这些化学成分的超声功率谱在癌变组织中比在正常组织中有更高的相关性,说明癌变组织的微观结构分布更一致。不同分类方法在肿瘤组织诊断中的准确率达到82%(优于临床标准方法)。因此,该技术显示了巨大的潜力,无痛早期诊断侵袭性前列腺癌。
该研究利用正常和癌变前列腺组织的光声理化谱建立前列腺癌诊断模型。基于UPGMA聚类分析方法分析了正常和癌变组织中不同大分子之间的相关性差异,并区分了不同生物大分子的特征光吸收波段V1-V6。发现,前列腺癌组织中血红蛋白、胶原蛋白和脂质的功率谱相关性明显高于正常组织,这反映了根据正常和肿瘤样本V1-V6可视化结果,这些生物分子分布的微结构相似性增加。这可能是因为复杂的肿瘤环境增加了光声谱的复杂性,使单一物质的分布特征变得模糊,从而增加了光声谱的相关性。这些结果表明,光声理化谱能有效反映肿瘤发展过程中生物大分子的变化,可用于前列腺癌的诊断。
该研究结果证明了将机器学习和光声理化光谱技术结合在探索前列腺癌微观结构和化学成分变化方面的可行性和有效性,从而促进前列腺癌的诊断。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Acoustic#
22
#OTOA#
32
#photo#
40
#机器#
29
前列腺癌相关研究,学习了,谢谢梅斯
46
学习了,谢谢分享
63