Annals of neurology:人类血液代谢组与阿尔茨海默病风险之间的关系
2022-08-25 Freeman MedSci原创
谷氨酰胺可能是预防和治疗AD的一个有希望的目标
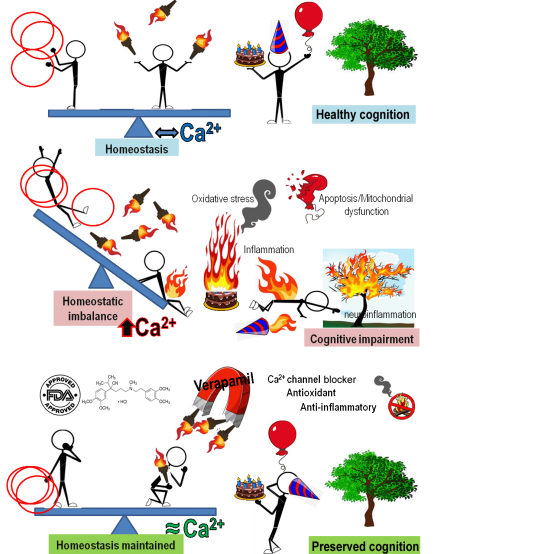
阿尔茨海默病(AD)是一种进行性的神经退行性疾病,影响到全世界大约5500万人。随着人口的增长和老龄化,AD的患病率将继续增长,并给世界各地的卫生保健系统带来越来越大的负担。令人失望的是,目前可用的AD药物治疗方法没有一种能够阻止或延缓AD症状的发展。
图1: 论文封面图
此外,最近研究和开发AD药物的临床试验也以失败告终。考虑到临床试验的巨大成本和药物开发的高损耗率,在临床试验之前探索牵涉到AD发生和发展的潜在生物标志物就显得尤为重要和紧迫。
人类的代谢组由内源性和外源性分子组成,代表了个人的代谢指纹。 鉴于代谢物与基因型和表型密切相关,代谢组学对于更清楚地阐明疾病的病理网络很有价值。Nelson等人报告说,有基因证据支持的与疾病相关的代谢物药物目标,获得市场批准的可能性是原来的两倍。
随着近年来质谱技术和高通量基因分型技术的空前发展,一些全基因组关联研究(GWASs)在揭示人类综合代谢组的遗传决定因素方面取得了巨大成就。因此,通过孟德尔随机化(MR)分析,整合遗传和代谢组学数据,可以准确地确定治疗AD的新的和有效的药物目标。
MR是一种新兴的方法,它使用遗传变异作为感兴趣的暴露的代理,以估计暴露和疾病之间的因果关系,而没有混杂或反向因果关系的偏差。MR设计先前已被用于评估某些生物标志物对AD风险的影响,包括系统性炎症调节剂、淀粉样蛋白和脂蛋白(a)。然而,到目前为止,还没有对人类代谢组进行系统扫描,以寻找有希望的AD因果介体。
为了填补这一空白,苏州大学的Lulu Sun等人首先对119种循环代谢物进行了系统的MR研究,以确定有希望的AD介体。在临床试验中测试潜在的药物靶点之前,可以应用全表型MR(Phe-MR)分析来揭示未预料到的不良反应,为药物再利用提供机会。因此,我们也对679个疾病特征进行了Phe-MR分析,以预测与代谢物干预相关的潜在靶点介导的副作用,以全面评估其临床安全性。
他们从3个代谢组全基因组关联研究(GWASs)中选择了119种独特的血液代谢物,有147,827名欧洲参与者。从国际阿尔茨海默病基因组学项目的63,926名欧洲人的GWAS荟萃分析中获得了有关AD的概要数据。
进行MR分析以评估血液代谢物与AD的关联,并进一步应用全表型MR分析以确定代谢物干预的潜在目标副作用。
四种代谢物被确定为AD的因果介导物,包括硫酸表雄酮(每SD增加的几率[OR]。0.60;95%置信区间[CI]。0.51-0.71;P=6.14×10-9),5α-雄性激素-3β-17β-二醇二硫酸酯(每SD增加的OR:0.69;95%CI:0.57-0.84;P=1. 98×10-4),鞘磷脂(每SD增加的OR:2.53;95% CI:1.78-3.59;P=2.10×10-7),和谷氨酰胺(每SD增加的OR:0.83;95% CI:0.77-0.89;P=2.09×10-6)。
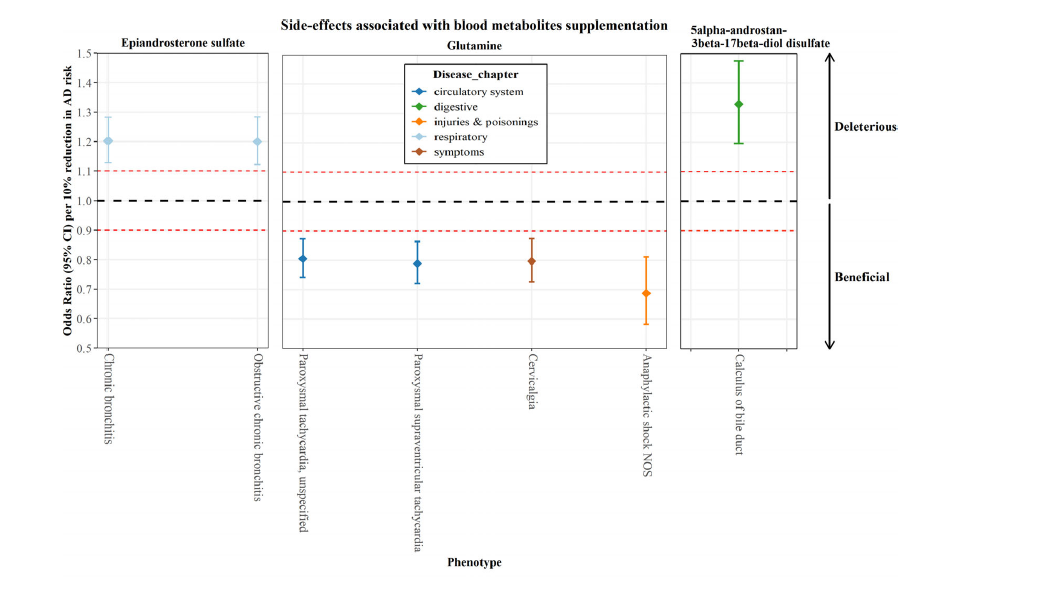
图2:论文结果图
MR分析显示,硫酸表雄酮、5α-雄烷-3β-17β-二醇二硫酸盐和鞘磷脂介导了多种疾病的风险,谷氨酰胺对4种疾病的风险有有益的影响。
该研究的重要意义在于发现了:从遗传学角度预测,硫酸表雄酮、5α-雄烷-3beta-17beta-二醇二硫酸盐和谷氨酰胺的增加可能与AD的风险降低有关,而鞘磷脂则与风险增加有关。副作用的特征有助于为药物目标的优先排序提供信息,谷氨酰胺可能是预防和治疗AD的一个有希望的目标,没有预测的有害的副作用。
原文出处:
Sun L, Guo D, Jia Y, et al. Association between Human Blood Metabolome and the Risk of Alzheimer’s Disease. _Annals of Neurology_. Published online August 15, 2022:ana.26464. doi:[10.1002/ana.26464](https://doi.org/10.1002/ana.26464)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
69
#血液代谢#
39
#阿尔茨海#
40
#阿尔茨#
42
#阿尔茨海默#
56
#代谢组#
43