茵栀黄注射液,这些年害了多少宝宝!
2016-09-07 小闪(整理 ) 医学论坛网
8月31日,国家食品药品监督管理总局在其官网上,发布了修改茵栀黄注射液说明书的公告,在禁忌项下标注“新生儿、婴幼儿禁用”!这已经足够引发各位粑粑麻麻的关注了,因为茵栀黄是最常用的新生儿退黄疸用药。茵栀黄注射液相关案例事实上,数年前网上就有关于茵栀黄注射液的新闻出现:2008年10月19日上午,卫生部召开紧急电视电话会议,通报了陕西省延安市志丹县医院因使用山西太行药业股份有限公司生产的茵栀黄注射液(
8月31日,国家食品药品监督管理总局在其官网上,发布了修改茵栀黄注射液说明书的公告,在禁忌项下标注“新生儿、婴幼儿禁用”!
这已经足够引发各位粑粑麻麻的关注了,因为茵栀黄是最常用的新生儿退黄疸用药。
茵栀黄注射液相关案例事实上,数年前网上就有关于茵栀黄注射液的新闻出现:
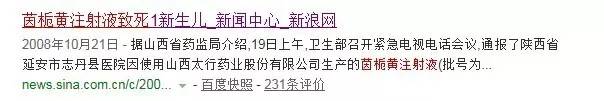
2008年10月19日上午,卫生部召开紧急电视电话会议,通报了陕西省延安市志丹县医院因使用山西太行药业股份有限公司生产的茵栀黄注射液(批号为071001)后,有4名新生儿发生不良反应,其中1名出生9天的新生儿于11日死亡。卫生部要求各地立即停止该批号茵栀黄注射液的临床使用。
茵栀黄是一种中药合剂,主要成分有茵陈、栀子、大黄、金银花,用于黄疸的退黄治疗。市面上的茵栀黄,有注射液、口服药、颗粒等多种类型。
虽然注射液禁用,但医院药房内仍有口服类型,大型药店也能买得到,网上不少急于给宝宝退黄的妈妈发帖求问,茵栀黄到底能吃吗?
同济医院新生儿科主任陈玲表示,茵栀黄对于生理性的黄疸,即正常发生的黄疸作用并不大。主要对于造成肝脏损伤的黄疸有作用。她建议家长根据宝宝情况,按医嘱服药,不要盲目,也不必恐慌。
微科普:
黄疸是新生儿最常见的症状,一般在新生儿出生的2~3天内开始表现出来,眼睛先黄,而后是面部变黄,从上而下到手、足,5~7天的黄疸数值达到最高,10天到两个礼拜左右,就会消退。
若生后24小时即出现黄疸,每日血清胆红素升高超过5mg/dl或每小时>0.5mg/dl;持续时间长,足月儿>2周,早产儿>4周仍不退,甚至继续加深加重或消退后重复出现或生后一周至数周内才开始出现黄疸,均为病理性黄疸。
治疗
1.光照疗法
是降低血清未结合胆红素简单而有效的方法。未结合胆红素经光照后可产生构形异构体、结构异构体和光氧化作用的产物,其中以结构异构体的形成最为重要,它能快速从胆汁和尿液中排泄而不需要通过肝脏代谢,是光疗降低血清总胆红素的主要原因。
目前国内最常用的是蓝光照射。将新生儿卧于光疗箱中,双眼用黑色眼罩保护,以免损伤视网膜,会阴、肛门部用尿布遮盖,其余均裸露。用单面光或双面光照射,持续2~48小时(一般不超过4天),可采用连续或间歇照射的方法,至胆红素下降到7毫克/分升以下即可停止治疗。
2.换血疗法
换血能有效地降低胆红素,换出已致敏的红细胞和减轻贫血。但换血需要一定的条件,亦可产生一些不良反应,故应严格掌握指征,一般用于光疗失败时。
3.药物治疗
应用药物减少胆红素的产生,加速胆红素的清除或抑制胆红素的肠肝循环,包括供应白蛋白,纠正代谢性酸中毒,肝酶诱导剂(如苯巴比妥),静脉使用免疫球蛋白。
4.支持治疗
主要是积极预防和治疗缺氧、高碳酸血症、寒冷损伤、饥饿、感染以及高渗药物输注等,防止血脑屏障暂时性开放,预防胆红素脑病的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#茵栀黄#
27
学习了,很有用。
62
学习了,很有用。
48
学习了,很有用。
57
很好的东东
55
成分复杂
57
学习学习。。。
23
#注射液#
26
#宝宝#
22
继续学习
28