病例分享:IVUS精准指导支架再狭窄治疗一例
2018-10-02 中国医科大学航空总医院 李邦合 董鹏 国际循环
随着腔内影像学(IVUS,OCT等)和功能学(FFR,iFR)的发展,我们可以在腔内影像学或功能学的指导下,优化PCI治疗,使治疗更趋于精准化,使靶病变能够选择应用最佳的治疗和尽可能改善预后的精准医疗,从而提高患者的生活质量和减少再次手术的病痛。针对该病例IVUS提供既往支架信息,判断支架内再狭窄可能原因及病变位置,更趋于精准化,从而指导本次手术策略,更大程度上优化PCI治疗,使患者获益最大化。
病例简介
患者,男,59岁,主因“间断胸痛、憋气3年,加重10余天”入院。患者于3年前间断出现胸痛、胸闷,多于活动后出现,无恶心、呕吐,无意识丧失,未有呼吸困难,咯血等不适。曾于当地医院诊断诊断“冠心病,不稳定型心绞痛”,后行冠状动脉造影+支架置入术,具体支架数目不详。术后恢复可,偶有胸痛,憋气,平素一般活动不受限。近10天前开始出现胸闷憋气症状,多于活动时出现,每次持续数分钟至数十分钟不等。既往否认高血压、糖尿病病史。有血脂高病史3年。
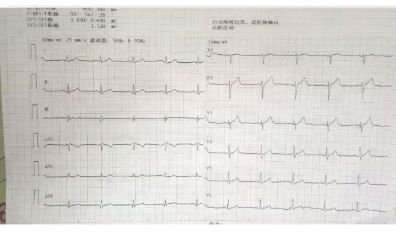
查体:BP 120/70 mm Hg,HR 70 bpm,心律齐,心音低钝,未闻及杂音。双肺(-),双下肢无水肿。辅助检查:心电图:窦性心律,心率80次/分,大致正常心电图;超声心动图结果:心脏结构与血流未见异常。化验:Tni<0.01 ng/ml,NT-proBNP 170 pg/ml。
诊断:1.冠状动脉粥样硬化性心脏病,PCI术后不稳定性心绞痛;2.高脂血症。
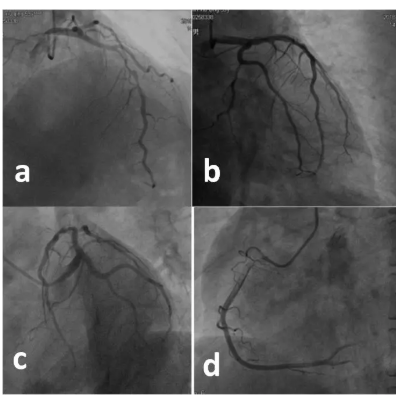
造影结果
①冠状动脉分布呈右优势型。
②LM(-),LAD p-m ISR 90%,D2p 80%,LCX(-),前向血流TIMI3级。RCA(-),前向血流TIMI3级。
③LADp-m,可见支架影,分支D2开口处狭窄约80%。
治疗策略
单支病变,患者家属拒绝CABG,可行PCI术。冠状动脉造影提示,左前降支可见支架影,支架内再狭窄(ISR),具体支架数目不清,是否衔接,衔接长度不清,再狭窄与支架的贴壁及支架的直径关系不清。考虑应用IVUS了解支架内结构情况,更好地指导治疗,确定远端病变是否需要补支架还是单纯药物球囊扩张治疗。
手术过程
1. 右桡动脉入径,7F EBU3.5,BHW送入主支、SION blue送入D1远端,沿主支导丝IVUS由支架远端至近端观察。
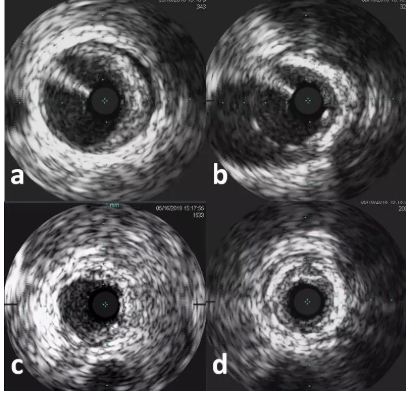
2. 沿D1支导丝掏网眼后IVUS观察角支。
3. 依据IVUS影像结果分析,主支支架内再狭窄,主支支架重叠部分位于D1开口后,主支支架外存在重度病变,病变长度约15 mm,主支支架丝覆盖D1开口,D1开口后存在中度狭窄。因此,策略制定为主支支架内再狭窄以药物球囊处理,支架外狭窄补支架一枚,角支开口扩张打开主支支架丝,D1开口至中段狭窄处扩张后以药物球囊处理。
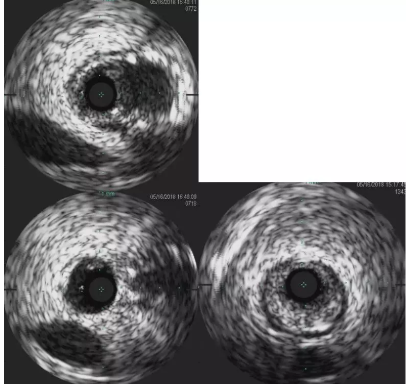
4. 手术过程:沿主支导丝送Tazuna2.0×15 mm扩张支架远端病变,支架内以Flextom2.5×6 mm 、Flextom3.0×10 mm扩张,后沿分支导丝送Tazuna2.0×15 mm、Flextom2.5×6 mm扩张,沿D1送入SeQuent2.5×20 mm扩张60 sec,沿主支近段支架内送SeQuent3.5×26 mm扩张60 sec,主支支架远端置入Integrity3.0×18 mm支架。
5. 术后影像

应用IVUS优化PCI治疗体会
随着腔内影像学(IVUS,OCT等)和功能学(FFR,iFR)的发展,我们可以在腔内影像学或功能学的指导下,优化PCI治疗,使治疗更趋于精准化,使靶病变能够选择应用最佳的治疗和尽可能改善预后的精准医疗,从而提高患者的生活质量和减少再次手术的病痛。针对该病例IVUS提供既往支架信息,判断支架内再狭窄可能原因及病变位置,更趋于精准化,从而指导本次手术策略,更大程度上优化PCI治疗,使患者获益最大化。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#精准#
34
#再狭窄#
47
学习了
64