Crit Care:基于肺形态的急性呼吸窘迫综合征患者一年结局
2022-06-04 MedSci原创 MedSci原创
肺形态反映了ARDS的急性期及其短期影响,但不反映长期结局,并且这只受合并症的影响。
急性呼吸窘迫综合征(ARDS)的死亡率自20世纪90年代末以来一直居高不下,没有下降的趋势。多种治疗方法未能提高急性呼吸窘迫综合征幸存者的生存率,其生活质量受到严重影响。急性呼吸窘迫综合征具有不同的表型和不同的短期预后。非局灶性ARDS患者的短期死亡率高于局灶性ARDS患者。近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,该研究的目的是评估ARDS形态学表型对患者长期预后的影响。
这项目是对LIVE研究进行的二次分析,该研究是一项前瞻性随机对照试验,根据中度至重度ARDS患者的肺形态来评估个性化呼吸机设置的有效性。ARDS分为局灶性(仅肺后下部的实变)和非局灶性病变。研究人员在1年的随访中使用死亡率和生活质量功能评分来评估患者结局。
该研究共纳入了124例局灶性ARDS患者和236例非局灶性ARDS患者。非局灶性ARDS患者的1年死亡率高于局灶性ARDS患者(37% vs 24%,p=0.012)。非局灶性ARDS(风险比为3.44;95%置信区间为1.80-6.59;p<0.001)、年龄、McCabe评分、血液系统癌症、SAPSII评分和肾替代治疗与1年死亡率独立相关。
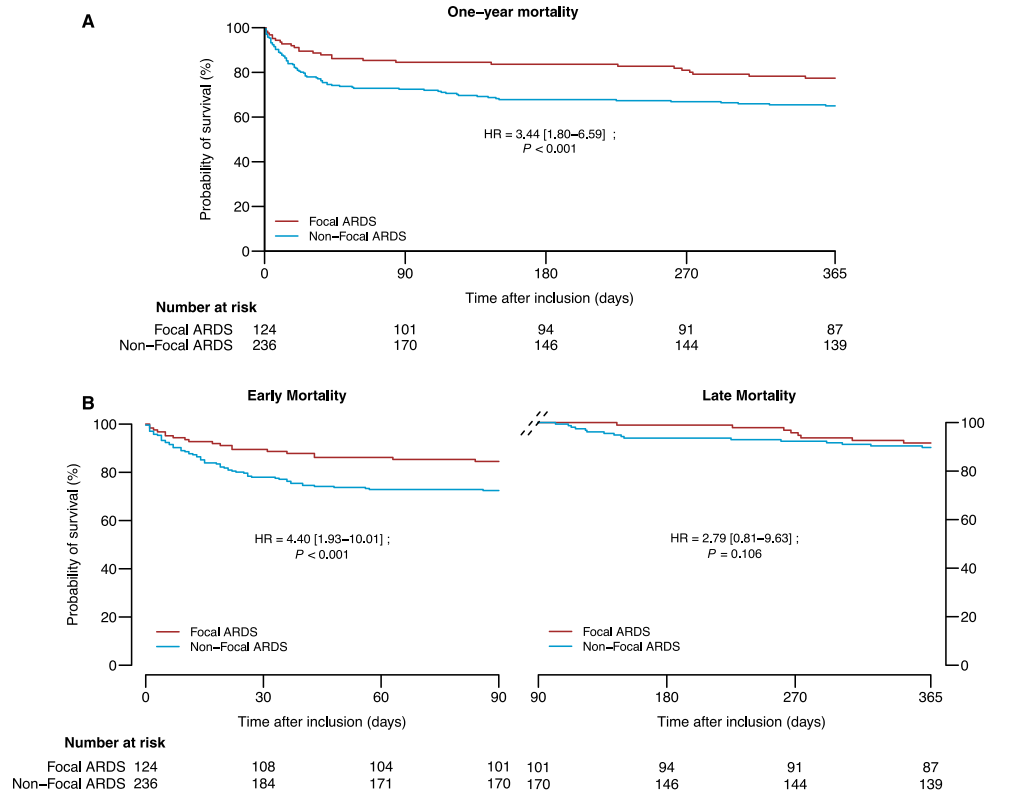
这种差异是由前90天的死亡率造成的(28 vs. 16%,p=0.010),但在90天到1年之间则不然(7 vs. 6%,p=0.591);此时,只有McCabe评分与死亡率独立相关。形态表型对患者报告的结局没有影响。
由此可见,肺形态反映了ARDS的急性期及其短期影响,但不反映长期结局,并且这只受合并症的影响。
原始出处:
Florian Blanchard,et al.One-year patient outcomes based on lung morphology in acute respiratory distress syndrome: secondary analysis of LIVE trial.Critical Care.2022.https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-04036-7#Sec7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#一年结局#
38
好
44
#综合征#
43
#呼吸窘迫#
40
学习了,谢谢分享
41