JACC:经导管肺动脉瓣置换术后心内膜炎的发生率、危险因素及预后
2021-08-07 Nebula MedSci原创
经导管肺动脉瓣置换术后心内膜炎的5年累积发生率为9.5%,8年累积发生率为16.9% ,每100人·年的年化发生率为2.2%
心内膜炎已成为经导管肺动脉瓣置换术(TPVR)后影响预后的最大不良事件之一。但是,目前关于这种并发症的危险因素和预后的数据有限。
本研究的目的是在一个大型多中心队列的TPVR后的患者中评估心内膜炎的危险因素和临床预后。
研究人员建立了一个国际注册中心,专注于TPVR后心内膜炎的特征,包括发生率、危险因素和临床预后。
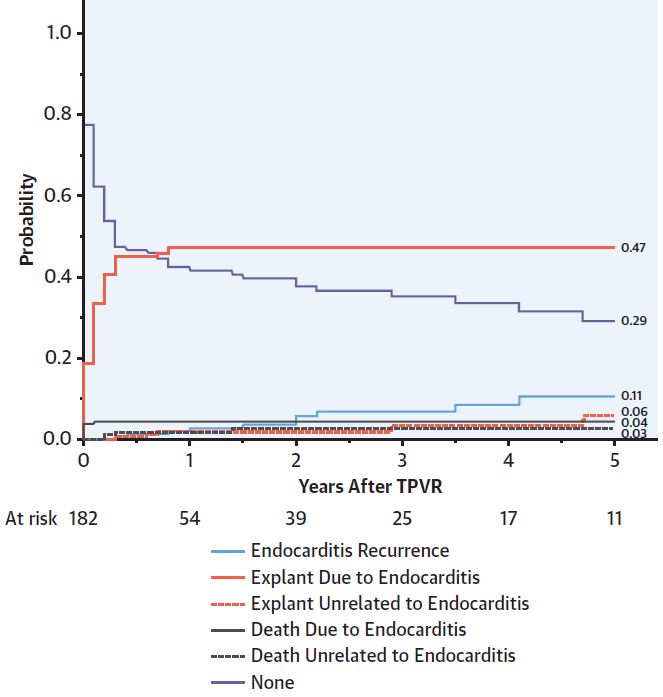
与心内膜炎、死亡/移植或非心内膜炎原因的再干预相关的任何类型TPV再干预的累积发生率
共纳入了2476位于2005年7月至2020年3月期间进行了TPVR的患者,共随访了8475个患者·年。总体上,在TPVR后中位随访了2.7年时,有182位患者确诊为心内膜炎,5年累积心内膜炎的发生率为9.5%(95%CI 7.9%-11.1%),8年累积发生率为16.9% (95%CI 14.2%-19.8%) ,每100人·年的年化发生率为2.2%。金黄色葡萄球菌和翠绿菌群链球菌共占心内膜炎病例的56%。
多变量分析证实,年龄较小、既往有心内膜炎史、残余梯度较高都是心内膜炎的危险因素,但在经导管肺动脉瓣型患者中无此相关性。总的来说,右心室流出道(RVOT)再介入治疗心内膜炎的发生率低于其他原因,但心内膜炎引起瓣膜移植发生率较高。
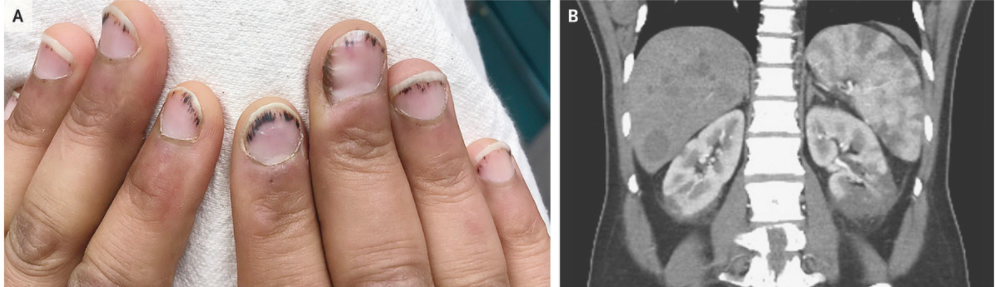
心内膜炎的各种预后发生情况
44%的患者为重度心内膜炎,其中12位患者(6.6%)死亡,几乎所有的都感染了金黄色葡萄球菌。
综上,在该多中心研究中,心内膜炎的发生率随时间的推移并不会发生明显的变化,与既往小规模的研究一致。该研究结果对于改善涉及RVOT的心脏病患者的生命周期管理至关重要。
原始出处:
Doff B. McElhinney, et al. Multicenter Study of Endocarditis After Transcatheter Pulmonary Valve Replacement. J Am Coll Cardiol. 2021 Aug, 78 (6) 575–589
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生率#
34
#肺动脉瓣#
28
#JACC#
41
#肺动脉瓣置换#
44
#置换#
33
#内膜#
34
很有用
52
#ACC#
0
#心内膜炎#
45
#经导管#
44