JNNP:多发性硬化:阿仑单抗治疗后视觉系统的结构和功能完整性
2021-07-10 MedSci原创 MedSci原创
多发性硬化(MS)是中枢神经系统(CNS)的一种炎症性脱髓鞘疾病。在大多数患者中,局灶性病变的累积以及灰质和白质萎缩的发展与进行性神经功能障碍的发展相关。MS药物可减少病变的累积和脑萎缩,但通常不会导
多发性硬化(MS)是中枢神经系统(CNS)的一种炎症性脱髓鞘疾病。在大多数患者中,局灶性病变的累积以及灰质和白质萎缩的发展与进行性神经功能障碍的发展相关。MS药物可减少病变的累积和脑萎缩,但通常不会导致残疾患者功能的持续改善。阿仑单抗是一种人源化抗CD52单克隆抗体,被批准用于治疗复发性多发性硬化症,可使活动性炎症疾病持续减少,并且在接受治疗的患者中,残疾状态量表(EDSS)评分的逐渐降低。虽然阿仑单抗的强大抗炎作用可能部分解释了早期的临床改善,脑萎缩率的长期益处和持续正常化提高了神经保护作用模式的可能性,并对包括再髓鞘化在内的恢复过程产生了影响。

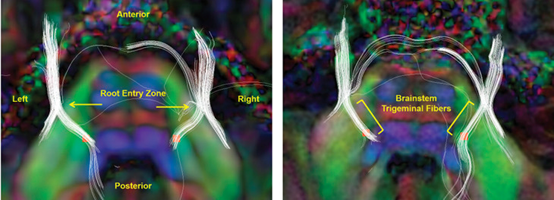
假设阿仑单抗治疗后持续的临床改善将反映在局部电生理和放射学指标的恢复上,特别是在MS中异常的电生理和放射学指标,慢性脱髓鞘MS病变内存活轴突的再髓鞘化证据支持这样一种观点,即阿来单抗治疗后观察到的残疾减少不能仅用抗炎作用来解释。视神经炎(ON)是检测治疗学的再髓鞘化潜能的最佳模型。在这种范式中,视觉诱发电位(VEP)的潜伏期被用作视神经髓鞘完整性/恢复的替代标记。由于VEP信号是在纹状体皮质水平产生的,其延迟反映了整个视觉通路(包括OR)的脱髓鞘程度。因此,多灶VEP(mfVEP)潜伏期延迟的恢复可能被用来监测视神经和OR病变内的髓鞘再生。病变限制性的径向扩散率(RD)增加与髓鞘丢失有关,至少在连贯的纤维束中提供了一个潜在的再髓鞘化生物标志物。本文以视觉通路为模型研究了阿来单抗的潜在神经保护和促再髓鞘化作用。
30名复发性多发性硬化症患者(McDonald 2010标准),按照治疗医生的处方开始服用阿仑单抗,在提供书面知情同意后被纳入研究。20名年龄匹配和性别匹配的健康对照者(HCs)被纳入参考组。神经系统评估,包括EDSS评分(仅限患者)和低对比度视力(Mars字母对比敏感度);mfVEP(澳大利亚悉尼VisonSearch);分别于基线、6个月、12个月和24个月时进行光学相干断层扫描(OCT)。 。使用TERRA软件(澳大利亚悉尼VisionSearch)测量每个时间点的平均mfVEP振幅和潜伏期;以及基线和24个月之间的潜伏期进展分析。简而言之,对于每只眼睛的每个节段(0-55),评估基线、12个月和24个月期间是否存在适当的VEP信号;使用TERRA软件,来自单个可读段的波形(即具有可检测振幅的波形)被自动映射到具有最大振幅的时间点的相应波形。在基线检查时、6个月、12个月和24个月时在3T GE MR750(美国威斯康星州密尔沃基通用电气公司)上获得MRI磁共振图像。使用半自动边缘检测轮廓技术,分别在FLAIR和T1对比后图像上测量T2病变。
患者和健康对照组的平均潜伏期变化
在患者中,观察到在整个研究过程中mfVEP潜伏期平均缩短1.21毫秒(95% CI 0.21至2.21,p=0.013),未因年龄、性别、病程或T2病变体积改变而改变。HC组的平均mfVEP潜伏期在研究过程中增加了0.72ms(不显著)。对慢性或T2病变(患者)的分析显示,在基线检查和24个月之间,标准化的各向异性分数和轴向扩散率增加(均p<0.01)。平均Mars字母对比敏感度在24个月时比基线时有所改善(p<0.001),并且受早期改善的驱动,患者和HC。虽然视觉系统提供了一个独特的机会来研究治疗的功能结构特异性效应,但我们的观察性研究确实强调了与未来2期再髓鞘化试验相关的一些考虑因素。在主要分析中,没有排除mfVEP潜伏期正常(<152 ms)的患者/眼睛,他们很可能具有正常的视觉通路传导,因此降低了研究对髓鞘再生的影响。
阿仑珠单抗治疗后有部分损伤再髓鞘化的迹象,视觉系统提供了一个独特的机会来研究治疗的功能结构特异性效应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#完整性#
50
#多发性#
45
#阿仑单抗#
39
#视觉#
48
学习了
55
好文章,谢谢分享。
65